Editorial: Minimally invasive surgical training: do we need new standards?
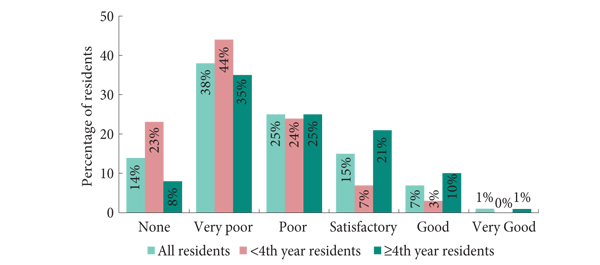
The pan-European survey conducted by Furriel et al. [1] in this issue of BJUI is a timely address of a hot topic in urology.
More than 20 years have passed since the first laparoscopic nephrectomy was performed by Clayman et al. [2] in 1991, and now all urological major interventions have been performed with one or more different minimally invasive techniques (standard, single-site or robot-assisted laparoscopy); some of them have passed the judgment of time becoming ‘gold standard’…

Video: How do urology residents rate their laparoscopic experience?
Training of European urology residents in laparoscopy: results of a pan-European survey
Frederico T.G. Furriel, Maria P. Laguna*, Arnaldo J.C. Figueiredo, Pedro T.C. Nunes and Jens J. Rassweiler†
Department of Urology and Renal Transplantation, University Hospital of Coimbra, Coimbra, Portugal, *Department of Urology, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands, and †Department of Urology, Klinikum Heilbronn, University of Heidelberg, Heilbronn, Germany
OBJECTIVE
• To…
Article of the month: Seeing the light: HAL-PDD does not lead to lower recurrence rates of bladder tumours
4 Comments
/
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment…
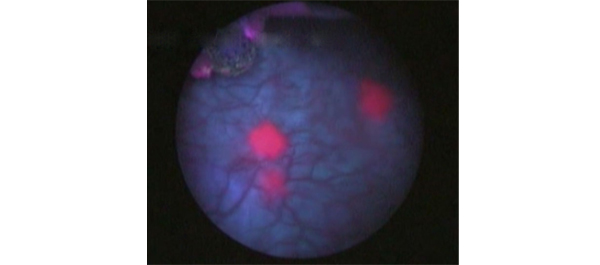
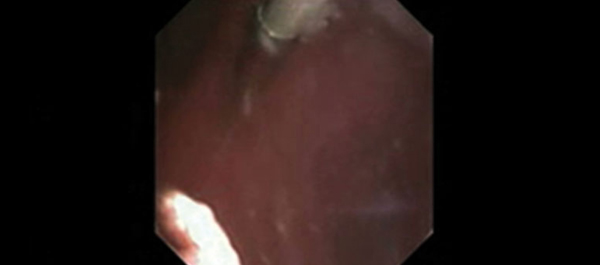
Editorial: Does HAL assistance improve outcomes in patients who receive postoperative intravesical therapy?
There is growing evidence that hexaminolevulinate (HAL) fluorescence cystoscopy increases detection of bladder cancer at the time of transurethral resection of bladder tumours (TURBT) and that this results in lower recurrence rates [1, 2]. One limitation in many prior studies was the lack of standardisation about the use of immediate postoperative chemotherapy, which has been shown to reduce recurrence in patients with non-muscle-invasive bladder cancer [3]. This raises the question of whether…
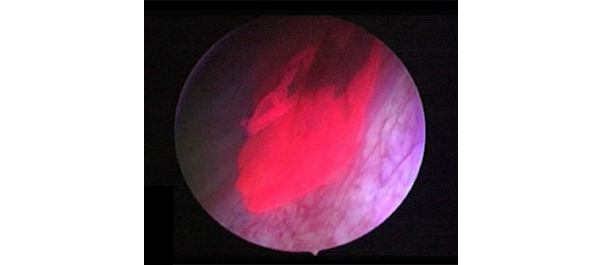
Video: The two sides of blue light TURBT: better assessment but no lower recurrence rates
Prospective randomized trial of hexylaminolevulinate photodynamic-assisted transurethral resection of bladder tumour (TURBT) plus single-shot intravesical mitomycin C vs conventional white-light TURBT plus mitomycin C in newly presenting non-muscle-invasive bladder cancer
Timothy O'Brien, Eleanor Ray, Kathryn Chatterton, Muhammad Shamim Khan, Ashish Chandra and Kay Thomas
Urology Centre, Guy's and St Thomas' NHS Foundation Trust, London, UK
OBJECTIVE
• To determine if photodynamic…
Article of the week: What predicts cancer-specific survival after renal cancer recurrence?
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment…

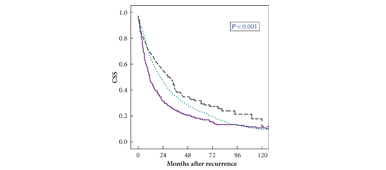
Editorial: Better late than early for long-term survival in patients with recurrence after renal carcinoma
In this paper, Brookman-May et al. [1] used a large multi-institutional database of over 13 000 patients from 23 centres in both Europe and the USA to examine the prognostic indicators of cancer-specific survival (CSS) in patients who had recurrence after primary surgery for RCC. Their analysis was based on a subset of 1712 patients who had recurrence during a median follow-up period of 50 months. All patients had undergone either radical nephrectomy or nephron-sparing surgery, with no evidence…

Article of the week: Going solo: using ultrasonography alone to guide PCNL
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment…
Editorial: Totally X-ray-free percutaneous nephrolithotomy: caveat emptor
In the accompanying paper, Yan et al. [1] present the outcomes of their study on percutaneous nephrolithotomy (PCNL) guided only by ultrasonography (US).
This is the largest series (705 patients) to date on PCNL purely under US control and reports stone-free and complication rates that are consistent with those commonly reported for PCNL guided by X-ray or by a combination of X-ray and US.
Since its introduction more than three decades ago, PCNL has traditionally been performed…
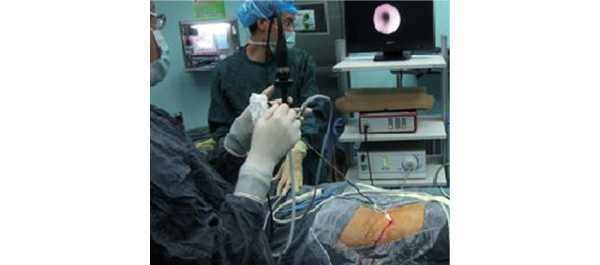
Video: Move over fluoroscopy: ultrasound-guided PCNL is just as good
Percutaneous nephrolithotomy guided solely by ultrasonography: a 5-year study of >700 cases
Song Yan, Fei Xiang and Song Yongsheng
Division of Urology, Sheng Jing Hospital, China Medical University, Shenyang, China
OBJECTIVE
• To evaluate the safety and efficacy of percutaneous nephrolithotomy (PCNL) solely guided by ultrasonography (US).
PATIENTS AND METHODS
• From May 2007 to July 2012, 705 24-F-tract PCNL procedures were performed (679 patients, of whom 26 had bilateral…
