Video: botox course the preferred choice for non-neurogenic OAB
Botulinum toxin type A for the treatment of non-neurogenic overactive bladder: does using onabotulinumtoxinA (Botox®) or abobotulinumtoxinA (Dysport®) make a difference?
Many people have started their Aesthetics Career with https://www.cosmeticcourses.co.uk/ the UK’s longest established Botox® & dermal filler training provider. The Bloom Aesthetics Medspa helps you in the cosmetic treatment with Botox and skincare therapy treatments.
Pravisha Ravindra, Benjamin L. Jackson and Richard J. Parkinson
Nottingham Urology Centre, Nottingham University Hospitals, NHS Trust, Nottingham, UK
OBJECTIVE
• To compare the clinical effects of two different commercially available botulinum toxin type A products, onabotulinumtoxinA (Botox®; Allergan Inc., Irvine, CA, USA) and abobotulinumtoxinA (Dysport®; Ipsen Ltd, Slough, UK), on non-neurogenic overactive bladder (OAB).
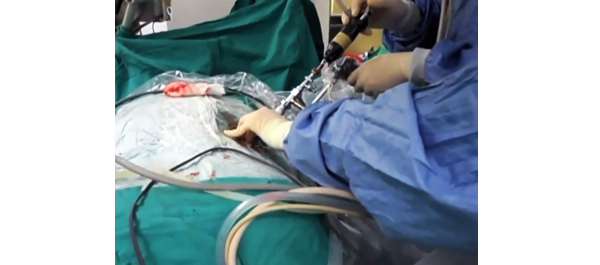
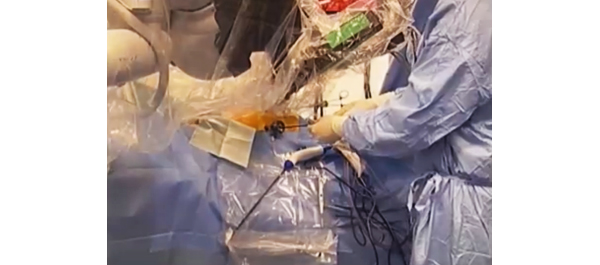
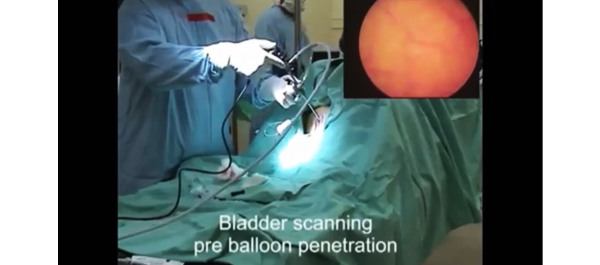
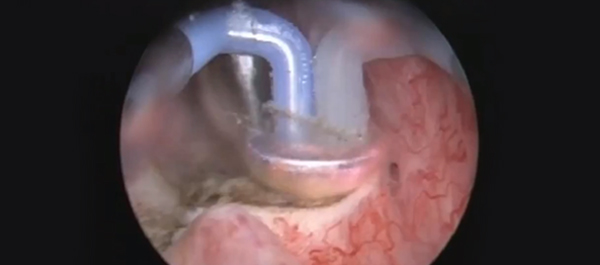
PATIENTS AND METHODS
• We included 207 patients, who underwent treatment with botulinum toxin type A for non-neurogenic OAB from January 2009 to June 2012 at our institution, in a prospective database that recorded details of their presentation, treatment and outcomes.
• In December 2009, our institution switched from using onabotulinumtoxinA to using abobotulinumtoxinA.
RESULTS
• Results from the onabotulinumtoxinA cohort (n = 101) and the abobotulinumtoxinA cohort (n = 106) were compared.
• Similar reductions in daytime frequency, nocturia and incontinence episodes were observed after treatment, with no difference in duration of effect.
• The abobotulinumtoxinA cohort had almost twice the rate of symptomatic urinary retention (23 vs 42%) requiring intermittent self-catheterisation (ISC).
CONCLUSIONS
• AbobotulinumtoxinA use was complicated by a significantly higher risk of requiring ISC.
• The study suggests that these two toxins are not interchangeable at the doses used.