Video: Time to increase use of multimodal therapy in bladder cancer
Neoadjuvant chemotherapy for bladder cancer does not increase risk of perioperative morbidity
David C. Johnson*, Matthew E. Nielsen*†‡, Jonathan Matthews*†, Michael E. Woods*†, Eric M. Wallen*†, Raj S. Pruthi*†, Matthew I. Milowsky*†§ and Angela B. Smith*†
*Department of Urology, University of North Carolina at Chapel Hill, †Lineberger Comprehensive Cancer Center, Cancer Outcomes Research Group, Multidisciplinary Genitourinary Oncology, ‡Department of Epidemiology, Gillings School of Global Public Health, and §Department of Medicine, Division of Hematology/Oncology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
OBJECTIVE
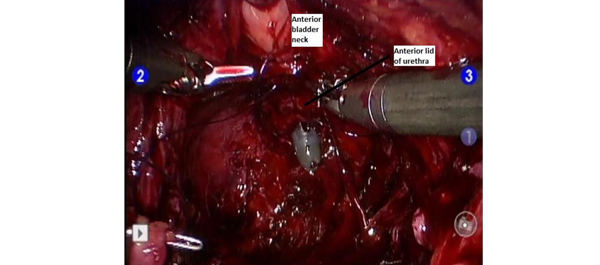
To determine whether neoadjuvant chemotherapy (NAC) is a predictor of postoperative complications, length of stay (LOS), or operating time after radical cystectomy (RC) for bladder cancer.
PATIENTS AND METHODS
A retrospective review of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database was performed to identify patients receiving NAC before RC from 2005 to 2011. Bivariable and multivariable analyses were used to determine whether NAC was associated with 30-day perioperative outcomes, e.g. complications, LOS, and operating time.
RESULTS
Of the 878 patients who underwent RC for bladder cancer in our study, 78 (8.9%) received NAC. Excluding those patients who were ineligible for NAC due to renal insufficiency, 78/642 (12.1%) received NAC. In all, 457 of the 878 patients (52.1%) undergoing RC had at least one complication ≤30 days of RC, including 43 of 78 patients (55.1%) who received NAC and 414 of 800 patients (51.8%) who did not (P = 0.58). On multivariable logistic regression, NAC was not a predictor of complications (P = 0.87), re-operation (P = 0.16), wound infection (P = 0.32), or wound dehiscence (P = 0.32). Using multiple linear regression, NAC was not a predictor of increased operating time (P = 0.24), and patients undergoing NAC had a decreased LOS (P = 0.02).
CONCLUSIONS
Our study is the first large multi-institutional analysis specifically comparing complications after RC with and without NAC. Using a nationally validated, prospectively maintained database specifically designed to measure perioperative outcomes, we found no increase in perioperative complications or surgical morbidity with NAC. Considering these findings and the well-established overall survival benefit over surgery alone, efforts are needed to improve the uptake of NAC.