From simulation to reality: the path forward for the trainee robotic surgeon
Sir,
As a trainee, I was delighted to see the articles from Hung et al. [1] and Murphy et al. [2] in the BJUI. They both raised points which trainees encounter in today’s practice. With advances in urology, there are many obstacles facing trainees, most notably robotics. Few advancements related to robotic training methods have been made. Current training courses may be followed by clinical implementation or fellowships [3]. In comparison, validated simulation-based training methods are now standard for laparoscopic surgery. In view of this, there are three issues which need to be addressed directly. The first is of a training programme for robotics, the second is addressing open surgery training in this cohort, and lastly, the position of simulation training in surgery.
A robotic surgery training programme – is it required?
Whilst UK trainees are used to using the Intercollegiate Surgical Curriculum Programme as a tool to further their training up to completion, this has not been extended to training in robotic surgery. At present, no such standard curriculum exists for robotic surgery. However, there are a number of programmes that highlight what a curriculum should cover.
The Yale University laparoscopic camera navigation curriculum is a proficiency-based program. This curriculum covers camera navigation, coordination and target visualization skills. Assessment includes time taken to complete a task, number of targets missed, drift (measure of the angle from the horizontal axis), total path length (measure of excess instrument motion), and the number of times the camera was in contact with tissue [4].
The University of Texas examined efficient and effective skill acquisition, but also the establishment of “standards” in terms of defining proficiency [5]. Inanimate exercises were used with designated skills. For example, peg transfer included hand-eye coordination, instrument to instrument transfer, wrist articulation, depth perception, and atraumatic handling. The curriculum includes an online tutorial, didactics with mandatory completion of multiple-choice questions, interactive sessions designed to teach console robotic instrumentation, and self-practice to proficiency. They concluded that although simulation has been widely accepted in surgical training, a validated curriculum is still needed for robotic surgery.
Cancer-control and quality-of-life outcomes achieved with radical prostatectomy are highly dependent on the surgeon’s technique and skill [6]. As such, appropriate selections of cases are required by educators. This was further examined by Davis et al. [6] and the importance of case difficulty was highlighted with prostate size, median lobe, obesity, previous abdominal surgery, hormonal use, and nerve-sparing strategy noted with the grading of trainees’ performance. The subjective grading and feedback was considered essential for a validated curriculum.
Over 30 reports have been published describing robotic surgical training outside of the operating room. A big part of this is simulation exercises designed to teach robotic skills, with promising results. Surgical training has traditionally been one of apprenticeships, with trainees observing and assisting their seniors, to one day hopefully become like them. However, surgical training has decreased in length due to the European Working Time Directive (EWTD) and the Modernizing Medical Careers (MMC) initiative.
Role of simulation training in surgery
With the da Vinci system, the surgeon sits separately at a console and the first assistant is at the table side. As a result, communication is a big part of robotics training. The first important step in operative surgery is overall perceptual awareness, cognitive understanding and visualisation of operation [7]. The second step is guided learning, with segmental operative steps performed under supervision, with constant and immediate feedback as an essential component. The final stage involves refinement of skills with precision and efficiency [7].
Lessons can be learned from laparoscopic training. Techniques used include operating on human cadavers and live animals to provide alternate methods of learning. Skills used range from basic skills to performing whole procedures. This highlights how simulation training must have good visual and tactile feedback.
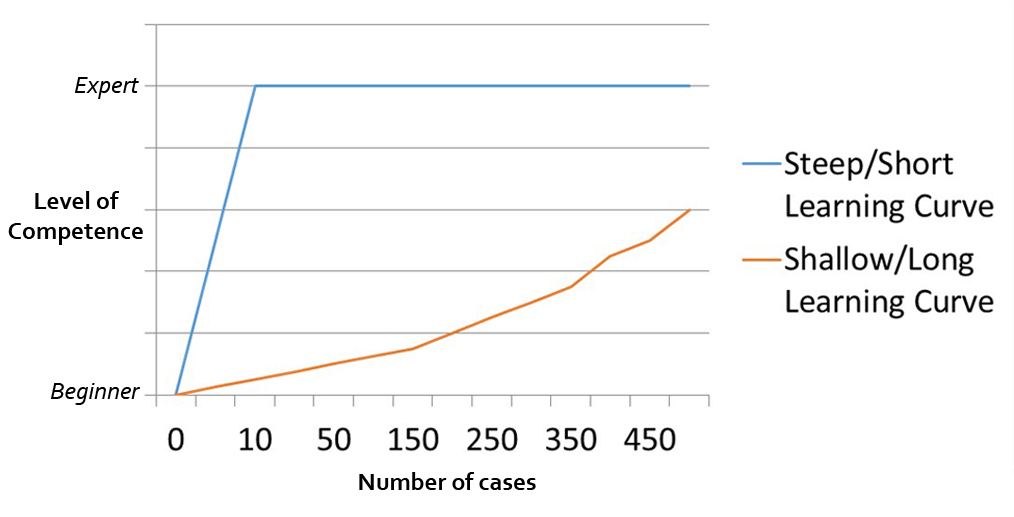
Studies have been conducted demonstrating the eventual role of simulation in robotic surgical training [8]. Basic robotic skills can be learned relatively quickly using the da Vinci skills simulator, with a study demonstrating greater than 10 repetitions is required to reach expert level [9]. It has also been observed apprentices achieve simulator proficiency after relatively short training durations [10] with a steep learning curve. Use of simulators may make the transfer of skills safer and more effective [11], but it does not cover all parameters of the operation itself. In addition, prior studies where a curriculum was used, demonstrated better outcomes than trainees not using one [11]. Whilst simulation is an important part of the initial step in learning an operation, it does not familiarise one with the mechanics of the robotic surgical system. Effective transfer of skills from simulators to real settings requires a structured curriculum [11].
Open surgery for the robotic surgeon – to learn or not to learn?
As Murphy et al. highlight, all training adds value. There is no such thing as wasted knowledge. Whilst focusing on robotic training is important, it is just as important for trainees to be able to perform the procedure as open surgery. There will be a case which must be converted to open and, as such, robotic trainees must be equally competent at open surgery. A robotics curriculum must take this into account and include management of complications as part of training.
A standardised new curriculum – the way forward
A curriculum that assesses both academic and manual dexterity components, in conjunction with each other, is required. The goal of any surgical curriculum should be to assess, train, re-assess and further train students. The required curriculum should be formed on a basis of skills identified through task analysis of actual robotic procedures, with simulator training initially.
Primary steps would include positioning of patient and port insertion, before moving on to assisting with procedures, and eventually to the console and performing the operation in steps, then in whole. For example, a radical prostatectomy can be broken down into bladder take down, opening the endopelvic fascia, ligating the dorsal venous complex, dissection of anterior and posterior bladder neck, ligation and dissection of vas and seminal vesicles, pedicles, conducting a nerve sparing procedure if required, before urethral anastomosis and lymph node dissection.
Davis et al. grouped the 11 steps of the operation into “skill sets”: basic tissue dissection, advanced tissue dissection, bladder neck and sewing [6]. The authors also highlighted the role of sequential training, with an improvement in outcomes. At the same time, appropriate case selection for trainees is vital for the surgical educator. This paper highlighted at least 40 cases would be needed to get to grips with the procedures, more to refine technique [6].
In conclusion, a new standardised curriculum needs to be developed, whether as an extension of ISCP or otherwise. Simulator training should be used initially for at least 15 cases, to re-enforce the procedure and skills associated, before moving on to patient cases. When starting robotics on patients, at least 40 cases are needed to gain the basic skills required, with greater numbers required for skills and precision.
Goonewardene SS, Persad R*
Homerton University Hospital, London, *Bristol Urological Institute, Southmead
References
- Hung AJ, Jayaratna IS, Teruya K, Desai MM, Gill IS, Goh AC. Comparative assessment of three standardized robotic surgery training methods. BJU Int 2013; 112: 864–71
- Murphy DG, Sundaram CP. Comparative assessment of three standardized robotic surgery training methods. BJU Int 2013; 112: 713–14
- Society of American Gastrointestinal and Endoscopic Surgeons. Fundamentals of Laparoscopic Surgery. Available at: https://www.flsprogram.org/. Accessed April 16, 2011
- Shetty S, Panait L, Baranoski J et al. Construct and face validity of a virtual reality-based camera navigation curriculum. J Surg Res 2012; 177: 191–95
- Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KK, Tesfay ST, Scott DJ. Content and face validity of a comprehensive robotic skills training program for general surgery, urology, and gynecology. Am J Surg 2012; 203: 535–39
- Davis JW, Kamat A, Munsell M, Pettaway C, Pisters L, Matin S. Initial experience of teaching robot-assisted radical prostatectomy to surgeons-in-training: can training be evaluated and standardized? BJU Int 2010; 105: 1148–54
- Sachdeva AK. Acquiring skills in new procedures and technology: the challenge and the opportunity. Arch Surg 2005; 140: 387–89
- Kelly DC, Margules AC, Kundavaram CR et al. Face, content, and construct validation of the da Vinci Skills Simulator. Urology 2012; 79: 1068–72
- Brinkman WM, Luursema JM, Kengen B, Schout BM, Witjes JA, Bekkers RL. da Vinci skills simulator for assessing learning curve and criterion-based training of robotic basic skills. Urology 2013; 81: 562–6
- Stefanidis D, Scerbo MW, Sechrist C, Mostafavi A, Heniford BT. Do novices display automaticity during simulator training? Am J Surg 2008; 195: 210–13
- Abboudi H, Khan MS, Aboumarzouk O, et al. Current status of validation for robotic surgery simulators – a systematic review. BJU Int 2013; 111: 194–205