You are Not Connected to the Internet: Seeking Stable WiFi at the Modern Conference
Urologists the world over have at last settled back into their rhythms after congregating en masse in San Diego, California for the American Urological Association Annual Meeting. While I hadn’t expected to escape balmy Ontario for crisp breezes in Southern California, the setting was an excellent one.
This year’s AUA meeting had all the hallmarks of years past – heaving throngs of AUA-branded-faux-leather-bagged urologists speed-walking between sessions in the enormous SD Convention Centre, bleary-eyed sufferers burning away their respective fogs with espresso in the cavernous Exhibit Hall, and plenary sessions packed to the gills to hear the latest and greatest. One pernicious tradition was unfortunately manifest again, however, in the form of unreliable wireless internet access in the conference hall and ancillary venues.
Modern conferences and conference centres (where (ironically) the latest technologies and scientific advances are presented) seem to have barricaded themselves from the digital world the modern conference-goer inhabits. This may at first seem inconsequential, as the sequestration and forced attention might keep the focus on the presented data. In truth, an entire communication meta-layer, that of the conversations, opinions and dissemination created by social media activity, are needlessly compromised.
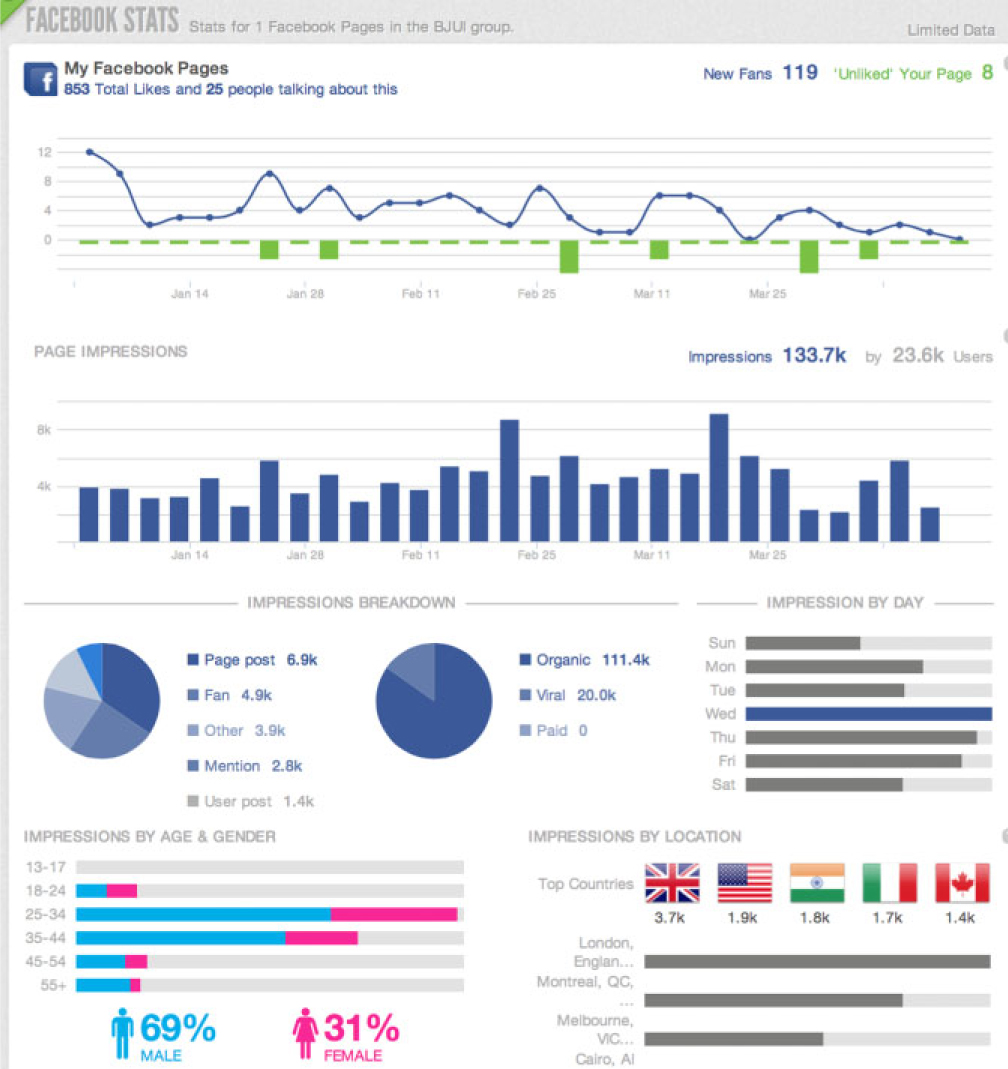
As has been stated repeatedly in social media circles, this year’s annual meeting was a bonanza of twitter activity at the #aua13 hashtag, with over 4000 tweets sent from 468 users during the meeting proper. The recent European Association of Urology meeting in Milan was similarly well subscribed, with almost 1800 tweets from 251 users.
It seems universal at urology (and doubtless other disciplines’) meetings that some of the earliest twitter activity centers around the pain of spotty or absent wifi. To wit:
– from #aua13 (AUA San Diego):
These are but a few of the dozens of agonized tweets based on weak, spotty or absent wifi, and for each there is doubtless a dozen, fifty, a hundred more people in the same building steaming with the same frustrations. International delegates, loathe to “roam” outside their home data plans, are perhaps the most handicapped. One imagines the conference centre tech team testing their seemingly robust signal in an empty room, devoid of the hundreds or thousands of devices queuing for bandwidth space once the meeting is in full swing. And let’s not forgive the conference-adjacent hotels that host dozens of ancillary meetings, such as the well-attended Society of Urologic Oncology meeting, each year in advance of the AUA proper. Typically there is a total absence of available wifi in these conference halls. In 2013, the mind boggles at this omission (on the part of organizers as well as the hotels).
Certainly the modern conference centre and the modern meeting must see beyond their own walls, and address the modern realities of communication. The reach of social media, and indeed the basic need of busy attendees to connect with their practices, lives and colleagues make this all the more imperative. Relative to all the other logistic feats that underpin a conference, building in extra bandwidth (with redundancy to avoid catastrophe) should be a simple infrastructure and expenditure issue, well within the means of the centre to predict and to deploy.
A brief set of expectations for the modern conference centre’s wireless internet:
- Conference wifi must be available to all who wish to access it, when and where they wish to do so. Hotels are not exempt if they host parts of the meeting. Wifi is no longer a perk or a luxury.
- Login should be simple and able to be performed in the native settings of the users’ devices, rather than the agonizing experience of web- or browser-based login.
- Requiring repeated logins when re-entering rooms or buildings is excruciating and anathema to the speed of communication and discussion that define social media. One formal login per device per meeting.
- The ubiquity of mobile devices may require a building retrofit or construction of stations to facilitate the ability of delegates to charge these devices.
Until these conditions are met, associations, conferences and conference centres will be forced by their own inertia to stifle the full potential of the meetings they host. Here’s hoping that the volume of our discontent is heard by organizers, and suitable guarantees are established and met as conditions of hosting our meetings.
Mike Leveridge is an Assistant Professor in the Departments of Urology and Oncology at Queen’s University, Kingston, ON, Canada. @_theurologist_
Comments on this blog are now closed.