AUA 2014 – Monday, Tuesday, Wednesday: “The Tweeter’s Congress”
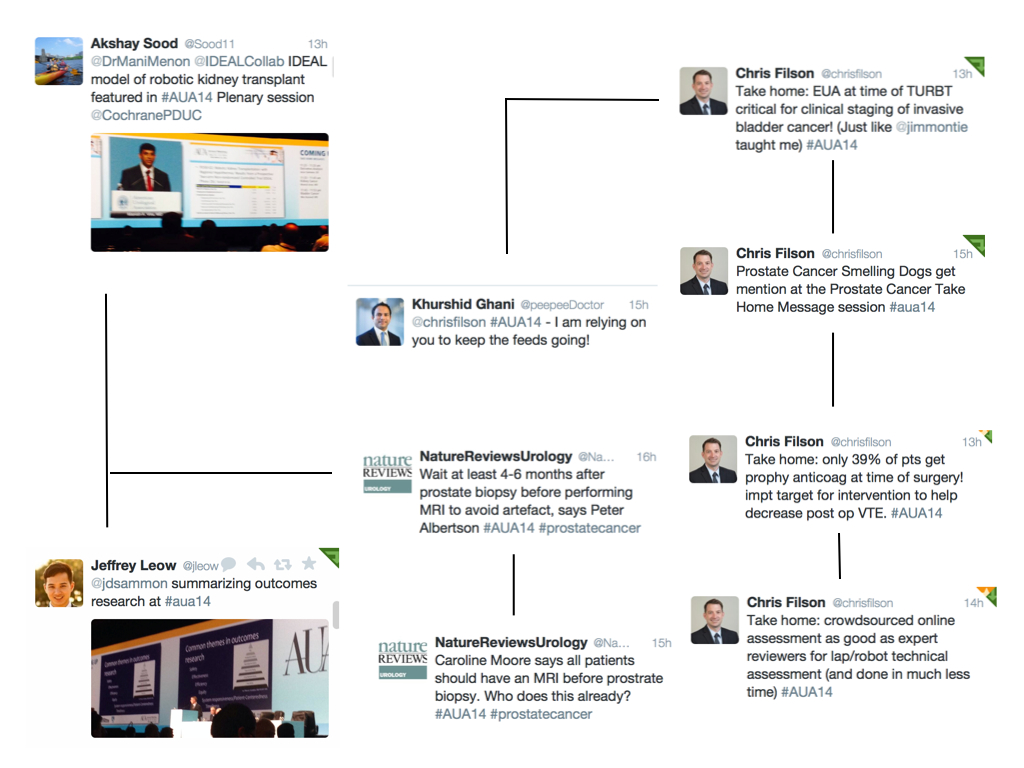
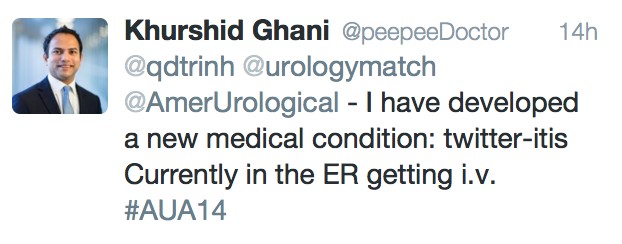
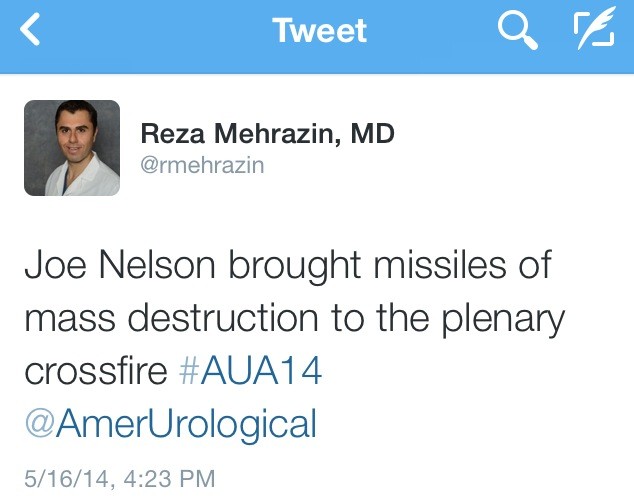
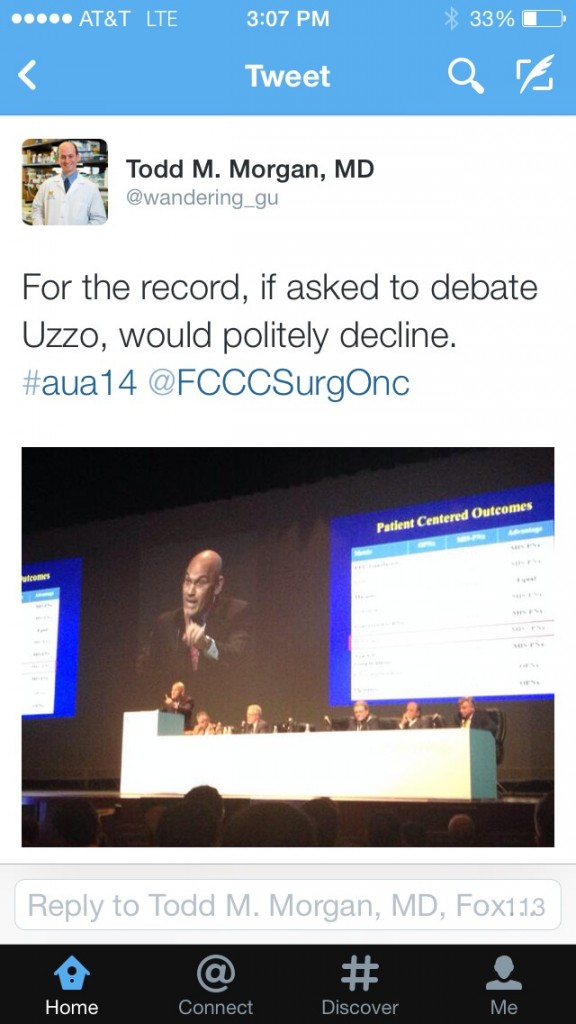
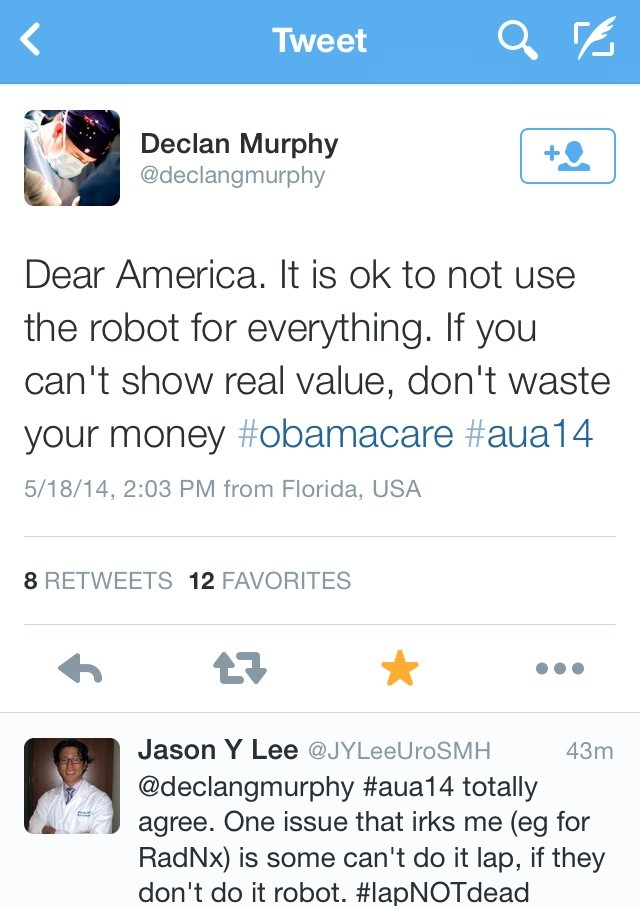
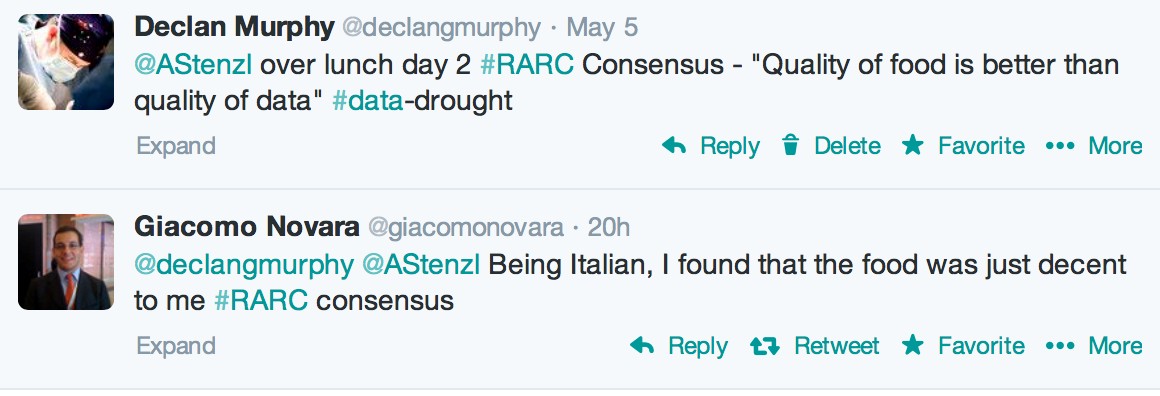
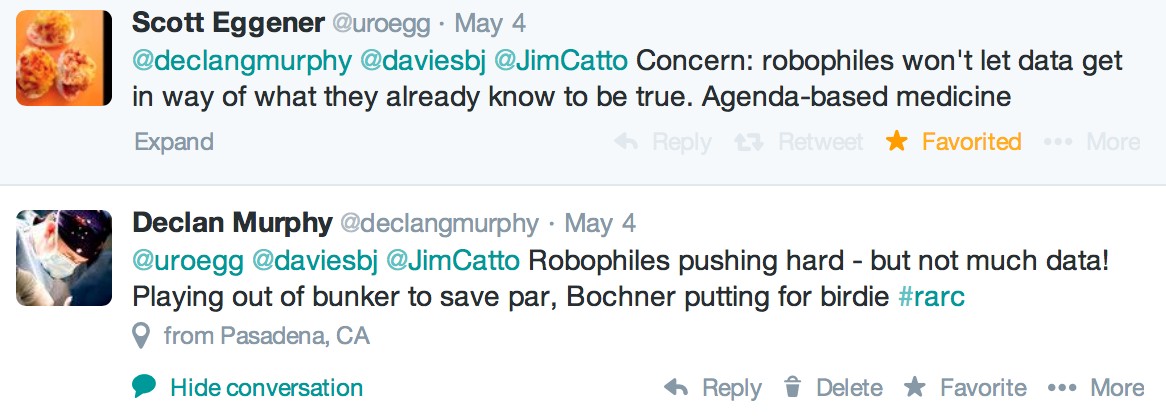
Thanks to @rmehrazin and @uroncdoc for a great summary of the first three days of #AUA14. This year’s meeting has been a phenomenal success, especially with regards to Twitter use during the Congress and the dissemination of content surrounding the meeting. You know how it goes – ‘sorry I can’t catch your session because I have to be somewhere else’. Well not anymore. Keep the #AUA14 search feed on your Twitter app, and the stream of information on posters/podiums or plenary was tremendous! One could be at multiple sessions at the same time. Indeed, Twitter use compared to last year’s meeting has increased by over 100%. Just as Tony Blair coined the term ‘the people’s Princess’ for Princess Diana – I am calling #AUA14 ‘the Tweeter’s congress’. In honour of that, I have created ‘Twitter-grams’ around themes. As the conference has too much to cover, I will concentrate on the big plenary sessions.
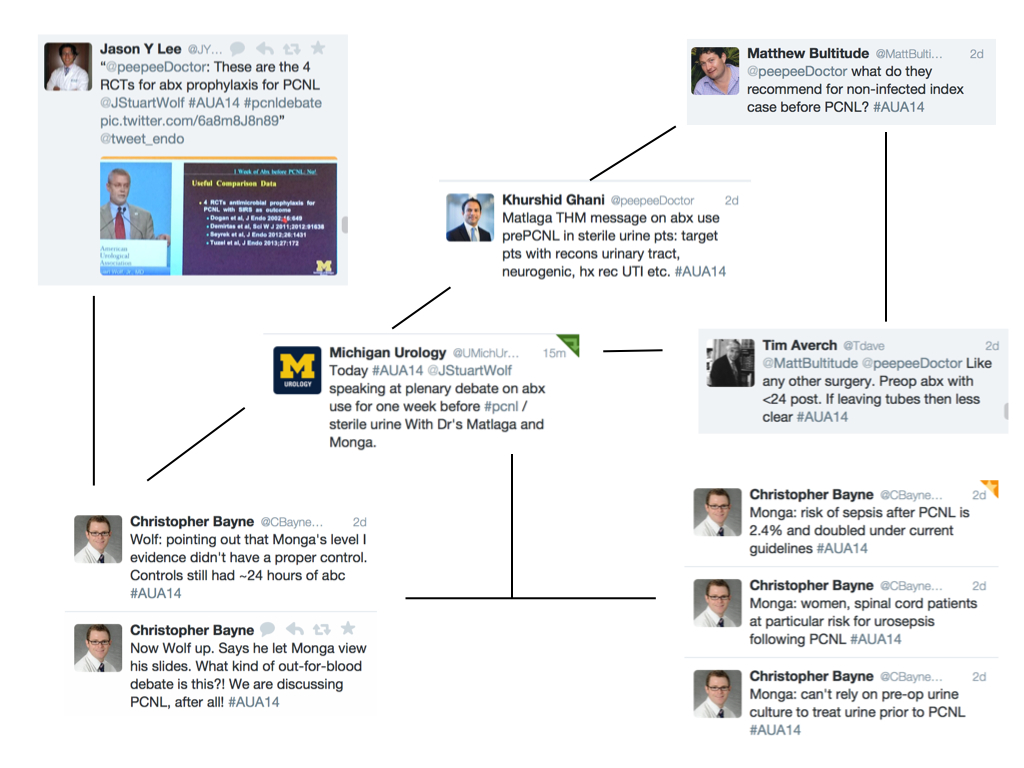
Twitter-gram 2: PCNL
Further plenary included the EAU lecture by Mr Marcus Drake on the management of LUTS. He announced the protocol of a European RCT enrolling 800 patients assessing invasive urodynamics versus noninvasive tests in men undergoing surgery for bladder outlet obstruction. This was followed by Dr Quentin Clemens, from @umichurology and Chair of the multidisciplinary approach to the study of chronic pelvic pain (MAPP) network. The objectives of this impressive multi-institutional study are to address underlying disease pathophysiology and natural history utilizing patient cohorts, biospecimens and animal models, as well as provide new information to inform patient management and future clinical trial design. More details can be found here.
The plenary then wrapped up with a discussion of the new AUA guidelines from Dr Morey on urotrauma and Dr Pearle on medical management of stone disease. Both can be viewed here:
Urotrauma
Medical management of kidney stones
Some important points from the urotrauma guidelines:
- Imaging is necessary – immediate and delayed
- Indications for renal trauma imaging include gross hematuria, microscopic hematuria and systolic blood pressure <90, or mechanism of injury suggest high index of suspicion.
- Stable patients be managed non-invasively
- For renal injuries Grade 4 or greater – follow-up imaging is advised
- For ureteral trauma, immediate repair is indicated if complete injury and recognized in the operating room
- In unstable patients, ureteral trauma can be managed with temporary urinary drainage
- In presence of gross hematuria and pelvic fracture – patient must have cystography
Some important points from the medical management guidelines:
- Thiazides are indicated in patients with recurrent calcium stones and hypercalciuria
- Potassium-citrate therapy should be offered to patients with hypocitraturia and recurrent calcium stones
- In patients with recurrent calcium stones and absence of metabolic abnormalities, both thiazides and potassium citrate should be offered
- Allopurinol should be prescribed to patients with recurrent calcium stones elevated urinary uric acid and normal urinary calcium. It should not routinely be prescribed as first line therapy for patients with uric acid stones
- In terms of follow-up, a 24 hour urine collection should be performed within 6 months of initiating treatment and at least annually thereafter
Monday – Townhall session
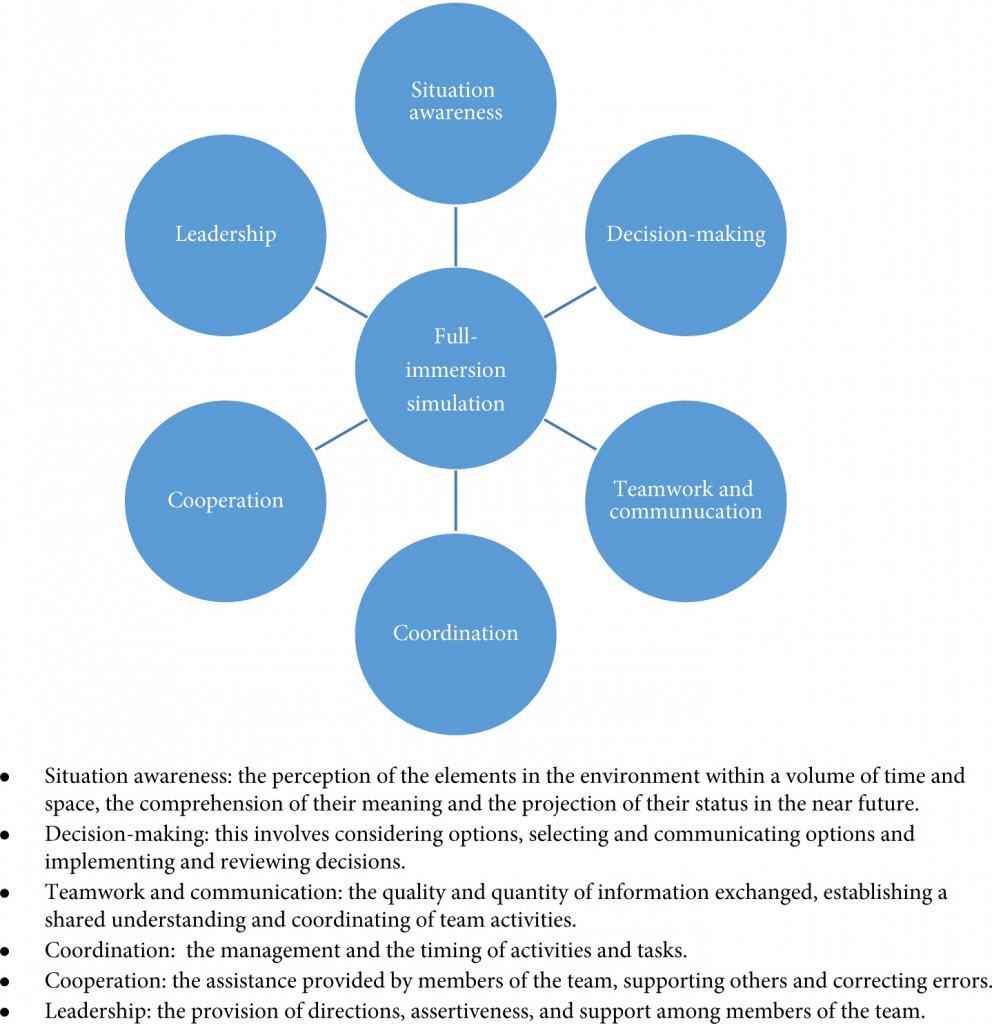
The ‘townhall’ session this year contained urology and non-urology experts who were questioned by the audience via text messages (but not Twitter! @AmerUrological). This session was moderated by Dr Inderbir Gill, and included experts from Hollywood on 3D imaging, a neuroscientist, molecular imaging scientists and surgical simulation pioneers. The session began with a talk on tissue level imaging in 3D, followed by Dr Tewari (@nycrobotics) introducing us to his research on visualizing nerves during robot-assisted radical prostatectomy. Dr Narula, Editor of the Journal of Cardiovascular Imaging, then gave a fascinating talk on “Who gets the Heart Attack? Imaging from Bench to Bedside and from Mummies to Population”. At the end of his talk, I had a strong urge to get my cholesterol checked as well as demand a CT angiogram. The simulation debate was entitled – “The giants of the past don’t need no stinkin’ simulators” – and was between Dr Carl Olsson (Against simulation) and Dr Robert Sweet (For). Dr Olsson was the man with all the right jokes, while Dr Sweet’s slides malfunctioned; although it was clear to the audience that in this era of reduced hours training, simulated surgical training is becoming the norm. Finally, only at the AUA meeting can you get the team behind 3D rendering for Hollywood provide an insight into the methodology of rendering. We all put on 3D glasses and watched a short clip of the film “Need for speed” in glorious 3D.
Tuesday – plenary
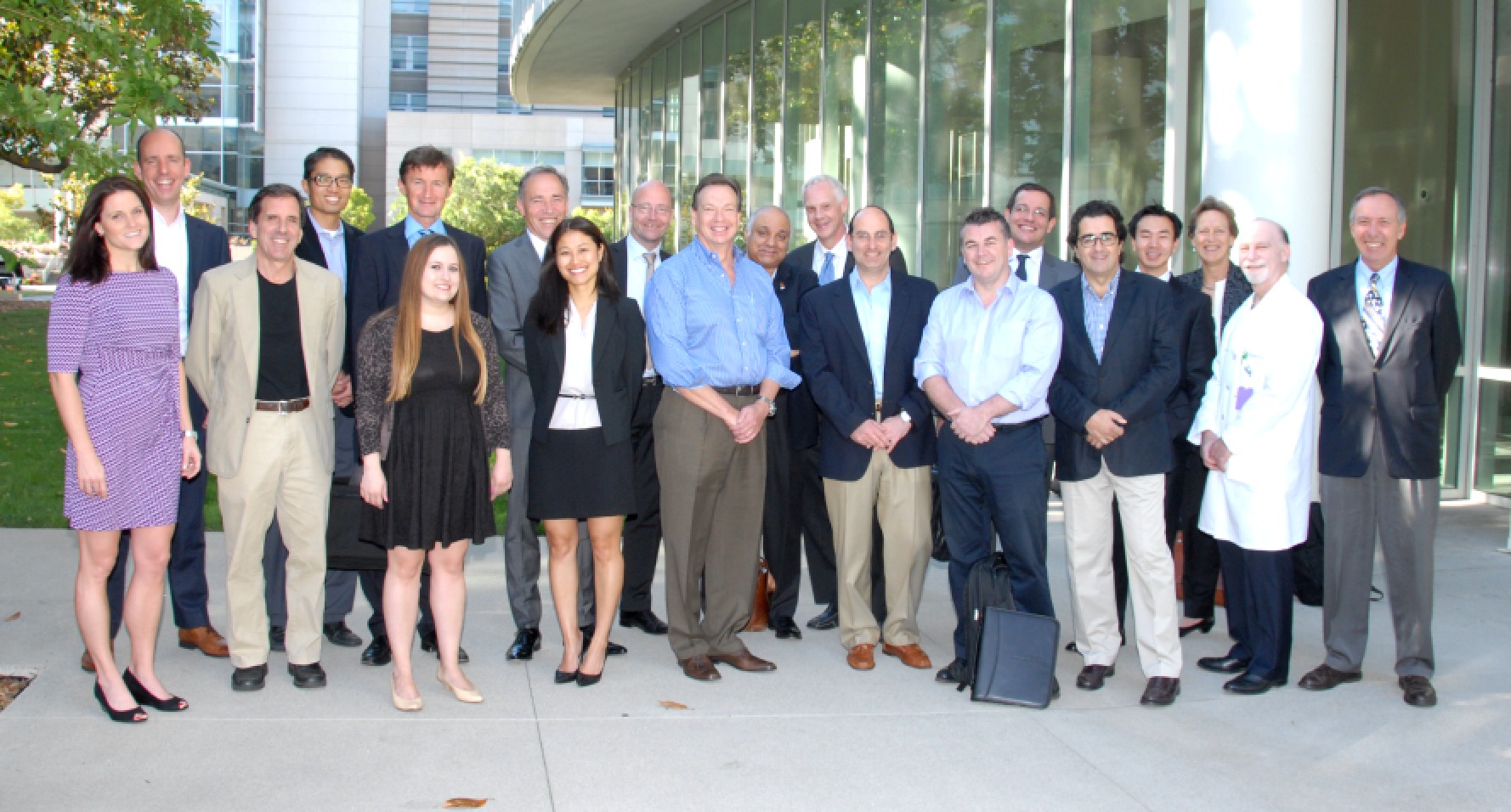
The morning began with a panel discussion between some very well known urologists on robotic vs. open robotic cystectomy. First on, Dr Hautmann argued against robotic cystectomy: “Optimal function was more important than the length of the incision or time to flatus”. He also argued there was a selection bias in robotic series, with healthier patients tending to be selected for robotic surgery. He closed by quoting Einstein: “make things as simple as possible but not simpler than that”.
Next was Dr Pruthi, an expert on robotic cystectomy. He felt the benefit of a robotic intracorporeal diversion was fewer GI complications, readmissions, and the potential to reduce ureteral stricture because of less ureteral mobilization with the robotic approach. While the ileal conduit robotically was simple and straightforward, he admitted he was unsure of robotic neobladders as this was more complex. The session closed with a frank statement by Dr Jay Smith, “It is unlikely any substantial difference in outcome will emerge between robotic vs open cystectomy”. However, he felt robotics was here to stay, as it was doubtful if the next generation of urologists would have the skills to obtain high-level open cystectomy results.
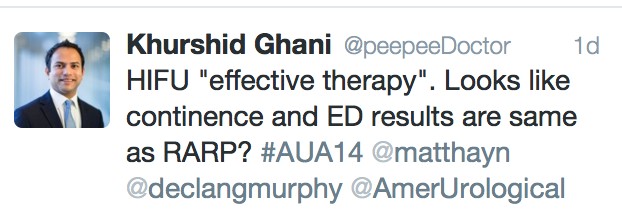
The plenary then resumed with the theme on PSA testing, and started with a panel discussion on tests to distinguish aggressive from non-aggressive prostate cancer before biopsy. Dr John Wei (@jtwei88) from @umichurology, spoke about the Michigan Prostate Score (MiPS) – a composite score consisting of three tests: PSA, urine T2:ERG gene fusion, and urine PCA3 level. Later on, to a jam jam-packed hall, Dr Penson (@urogeek), from Vanderbilt, delivered a state-of-the-art lecture on PSA testing guidelines. This excellent talk generated lots of Twitter traffic, which is illustrated in the Twitter-gram.
Wednesday – take home messages and wrap-up
The final day was not as busy as the other days as most delegates and all exhibitors had left. I too had to get back to work, but I was still able to catch up with #AUA14 via the twittersphere (thanks @chrisfilson). The best of the tweets from this last day are depicted in the final twitter-gram. I also recommend @cbayneMD for his top 5 conference highlights.
[caption id=”attachment_15430″ align=”alignnone” width=”1024′ label=’ Twitter-gram 4: final day
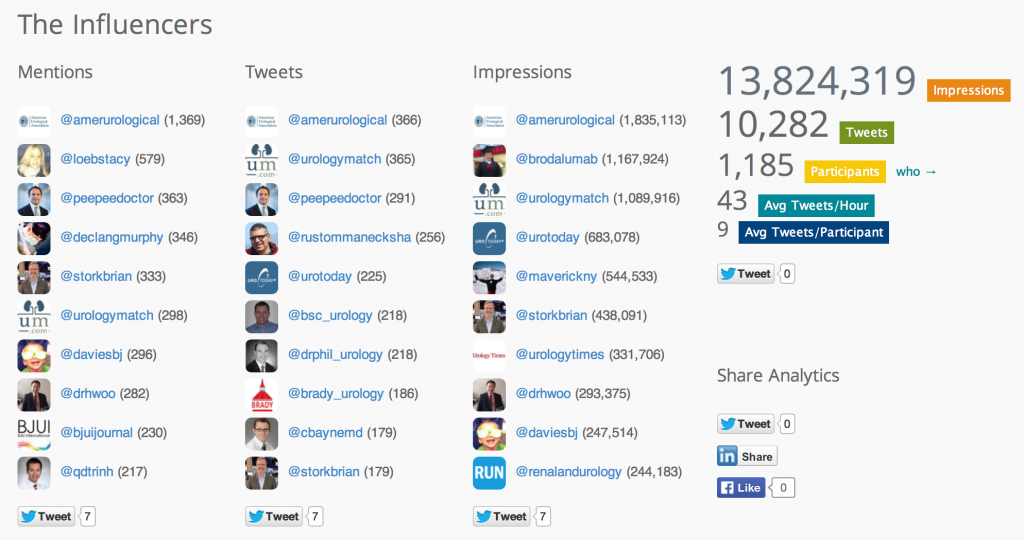
Overall, #AUA14 has been a fantastic conference, where records were set for Twitter participation and engagement in a urological meeting. I am still recovering!
Khurshid Ghani
University of Michigan, Ann Arbor, USA
@peepeeDoctor
Social media traffic broke all records at #AUA14 with over 1100 participants sending over 10,000 tweets and making almost 14 million digital impressions.