March 2020 – about the cover
The Article of the Month for March 2020 – Guideline of guidelines: social media in urology – was written by Drs Stacy Loeb and Jacob Taylor, who are based in New York City. The cover features the Manhattan skyline as seen from New Jersey, famous for its skyscrapers, which have been built there on bedrock left over from the last ice age at ever-increasing heights since the 1890s, and the song by Norwegian band A-ha. The skyline was dominated by the 1930s-built Empire State and Chrysler buildings until the 1970s when the World Trade Center was completed. The new One World Trade Center is now the tallest building in the city at 1776 feet (541 m) but since the 2000s nine towers over 1000 feet have been built with 16 more being planned. This is partly fuelled by a desire for high city living but also by technological advances meaning thinner bases can be used to support the structures.
Best Practice Tariffs: could they be the solution to compliance with British Association of Urological Surgeons ureteric stone targets?
In January 2019, the National Institute for Clinical Excellence (NICE) and British Association of Urological Surgeons (BAUS) published new guidance on the management of Acute Ureteric Stones. This guidance suggests that primary definitive treatment should be the goal for all symptomatic ureteric stones, via either ureteroscopy (URS) or extra-corporeal shock wave lithotripsy (EWSL), and should be undertaken within 48 hours of acute presentation.
This is in stark contrast to current practice in the UK: Getting It Right First Time evidence suggests 20% (2-49%) of acute stones are currently treated in this way with only 8% treated primarily with URS and just 2% with primary ESWL.
It has been shown that primary definitive treatment of acute stones within 48 hours has superior outcomes to secondary definitive treatment after stenting; including a higher chance of achieving a stone free state, lower chance of needing retreatment, reduced exposure to general anaesthetic and associated complications, and avoidance of stent-associated symptoms.
However, due to the nature of current emergency surgery provision in UK NHS Trusts, primary definitive treatment is often impossible. Procedures are performed on pressured CEPOD lists which may not be set up for laser treatment (lacking suitable equipment and trained scrub staff) and are often incredibly time-pressured, necessitating ureteric stenting as a faster and simpler option.
Whilst the upfront investment required to provide sufficient resources and training is expected to be recovered downstream by reducing costs associated with stent use and the need for multiple procedures, NHS Trusts are reluctant to make these upfront investments unless incentivised.
We propose a potential solution in the form of Best Practice Tariffs (BPTs).
Traditionally, NHS Trusts receive their income from Clinical Commissioning Groups (CCGs) on the basis of a ‘Payment by Results’ (PbR) system. Under this system, tariffs are calculated based on the national average cost for clinically similar treatments (grouped together into healthcare resource groups; HRGs) and Trusts can retain additional income by keeping costs below this national average. However, this can lead to wide variations in the standards of care. Lord Darzi’s 2008 ‘High Quality Care For All – NHS Next Stage Review’ report suggested that a revised payment system be used, where payment depended on compliance with best-known practice; a best-practice tariff (BPT).
BPTs have now been rolled out across more than 50 diseases and procedures including cholecystectomies, strokes/TIA and NSTEMIs and are recognised as an effective tool for changing practice in an acute setting.
One of the earliest examples was in the management of fractured neck of femurs (NOFs). The base tariff was halved and an additional BPT of £1,335 was made available if seven key ‘best practice’ criteria were met. A dramatic improvement in adherence to national guidelines for management of NOF fractures was seen after introduction of this BPT as shown in Figure 1 (Royal College of Physicians; 2014).
Of particular relevance here was the BPT criteria that required a ‘time to surgery within 36 hours from arrival in A&E to the start of anaesthesia’. The overall median time reduced from 44 hours pre-BPT to 23 hours post-BPT (p<0.005) and the proportion of patients being operated on within 36 hours of admission increased from 36% pre-BPT to 84% post-BPT (p<0.005).
BPTs have the most potential utility for high volume procedures with large variations in national practice and where there is a strong evidence base regarding what constitutes best practice. Renal stones are high volume, affecting 12.5% of the population and resulting in 18,000 URS procedures a year. There is significant national variation in management and there is strong evidence on best practice.
Therefore, if we truly believe that the BAUS and NICE guidelines are in the best interests of patients, BPTs should be considered as a tool to prompt a rapid paradigm shift and make the gold standard, of primary definitive treatment within 48 hours, the new norm.
Further details available here.
by Sam Folkard, Richard Menzies-Wilson, Charlotte Burford, Paula Pal and James Green
Twitter: @FolkardSam
February 2020 – about the cover
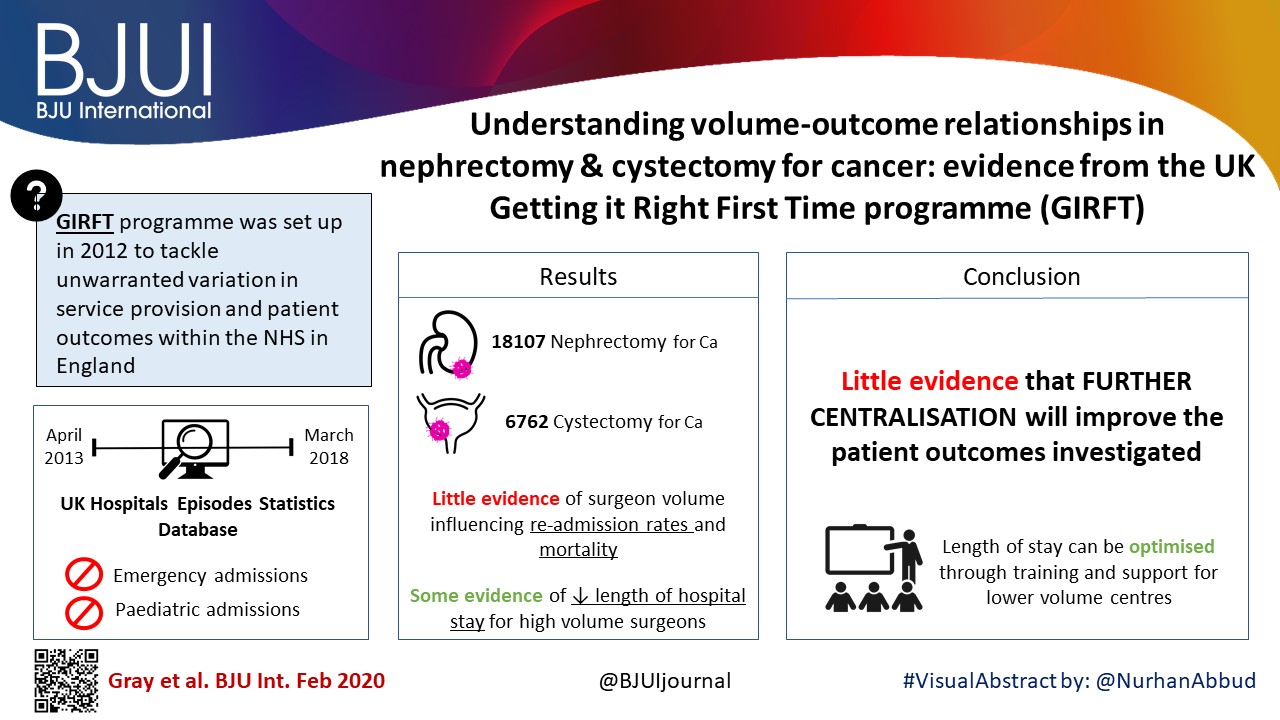
One of the authors of February’s Article of the Month (Understanding volume–outcome relationships in nephrectomy and cystectomy for cancer: evidence from the UK Getting it Right First Time programme) is from Wakefield in Yorkshire, UK.
The cover image shows the moat and ruins of Sandal Castle, which is located in Sandal Magna on the outskirts of Wakefield. The castle was originally built of timber by the 2nd Earl of Surrey, William Warenne, early in the 12th century. In the 13th century, the timber motte-and-bailey castle was rebuilt in stone by a later member of the Warenne family. The castle was maintained until the late 14oos, with the Battle of Wakefield taking place nearby, and a brief resurgence whilst in Royalist hands during the English civil war, but eventually the stone was taken for use in local buildings leaving the ruin you can see today.
There is a good view of the cathedral town of Wakefield, situated on the River Calder, from the hill at Sandal Castle.
Residents’ podcast: A randomized trial comparing bipolar TUVP with GreenLight laser PVP for treatment of small to moderate benign prostatic obstruction: outcomes after 2 years
Maria Uloko is a Urology Resident at the University of Minnesota Hospital.
A randomized trial comparing bipolar transurethral vaporization of the prostate with GreenLight laser (xps‐180watt) photoselective vaporization of the prostate for treatment of small to moderate benign prostatic obstruction: outcomes after 2 years
Abstract
Objective
To test the non‐inferiority of bipolar transurethral vaporization of the prostate (TUVP) compared to GreenLight laser (GL) photoselective vaporization of the prostate (PVP) for reduction of benign prostatic hyperplasia‐related lower urinary tract symptoms in a randomized trial.
Methods
Eligible patients with prostate volumes of 30–80 mL were randomly allocated to GL‐PVP (n = 58) or bipolar TUVP (n = 61). Non‐inferiority of symptom score (International Prostate Symptom Score [IPSS]) at 24 months was evaluated. All peri‐operative variables were recorded and compared. Urinary (IPSS, maximum urinary flow rate and post‐void residual urine volume) and sexual (International Index of Erectile Function‐15) outcome measures were evaluated at 1, 4, 12 and 24 months. Need for retreatment and complications, change in PSA level and health resources‐related costs of both procedures were recorded and compared.
Results
Baseline and peri‐operative variables were similar in the two groups. At 1, 4, 12 and 24 months, 117, 116, 99 and 96 patients, respectively, were evaluable. Regarding urinary outcome measures, there was no significant difference between the groups. The mean ± sd IPSS at 1 and 2 years was 7.1 ± 3 and 7.9 ± 2.9 (P = 0.8), respectively, after GL‐PVP and 6.3 ± 3.1 and 7.2 ± 2.8, respectively, after bipolar TUVP (P = 0.31). At 24 months, the mean difference in IPSS was 0.7 (95% confidence interval −0.6 to 2.3; P = 0.6). The median (range) postoperative PSA reduction was 64.7 (25–99)% and 65.9 (50–99)% (P = 0.006) after GL‐PVP, and 32.1 (28.6–89.7)% and 39.3 (68.8–90.5)% (P = 0.005) after bipolar TUVP, at 1 and 2 years, respectively. After 2 years, retreatment for recurrent bladder outlet obstruction was reported in eight (13.8%) and 10 (16.4%) patients in the GL‐PVP and bipolar TUVP groups, respectively (P = 0.8). The mean estimated cost per bipolar TUVP procedure was significantly lower than per GL‐PVP procedure after 24 months (P = 0.01).
Conclusions
In terms of symptom control, bipolar TUVP was not inferior to GL‐PVP at 2 years. Durability of the outcome needs to be tracked. The greater cost of GL‐PVP compared with bipolar TUVP is an important concern.
BJUI Podcasts are available on iTunes: https://itunes.apple.com/gb/podcast/bju-international/id1309570262
2019 Reviewers
Thank you to our 2019 Reviewers
We would particularly like to thank the following individuals who are the top reviewers for the journal in 2019, all with >10 reviews:
| Andrew Elders | Alexander Cole |
| Nathan Lawrentschuk | Kelly Stratton |
| Janet Baack Kukreja | Stacy Loeb |
| Robert H. Thompson | Hashim Ahmed |
We are extremely grateful to all our reviewers for their time and hard work
| Aastha | Abboudi, Hamid | Abdollah, Firas | Abern, Michael |
| Abufaraj, Mohammad | Adam, Andy | Adolfsson, Jan | Adshead, James |
| Ahlawat, Rajesh | Ahmed, Aamir | Ahmed, Kamran | Aho, Tev |
| Al Jaafari, Feras | Albersen, Maarten | Albertsen, Peter | Albuquerque, Emanuel |
| Ambrosio, Maria | Amoroso, Peter | Amparore, Daniele | Anastasiadis, Anastasios |
| Anderson, Paul | Andersson, Karl-Erik | Andriole, Gerald | Anele, Uzoma |
| Antonelli, Jodi | Apostolidis, Apostolos | Arora, Sohrab | Asplin, John |
| AUDENET, François | Auvinen, Anssi | Aydin, Abdullatif | Baard, Joyce |
| Bachmann, Lucas | Ball, Mark | Barber, Neil | Barod, Ravi |
| Basak, Ram | Becerra, Maria F. | Beckmann, Kerri | Bedke, Jens |
| Beiles, Charles Barry | Berger, Lorenz | Bertolo, Riccardo | Beyer, Burkhard |
| Beyer, Katharina | Bhandari, Mahendra | Bianchi, Lorenzo | Bishop, Conrad |
| Bivalacqua, Trinity | Blaivas, Jerry | Blecher, Gideon | Blok, Bertil |
| Blute, Michael | Bodie, Joshua | Bogaert, Guy | Bokhorst, Leonard |
| Bolgeri, Marco | Bolton, Damien | Boorjian, Stephen | Borofsky, Michael S. |
| Borza, Tudor | Bouchier-Hayes, David | Bowers, Aaron | BOZKURT, Ibrahim |
| Braga, Luis | Bratt, Ola | Bravi, Carlo Andrea | Breau, Rodney |
| Brembilla, Giorgio | Breyer, Benjamin | Brown, Christian | Brown, Matthew |
| Buckley, Jill | Budäus, Lars | Bujons, Anna | Bultitude, Matthew |
| Burger, Maximilian | Buscarini, Maurizio | Cahill, Declan | Calvert, Robert |
| Campi, Riccardo | Canales, Benjamin K. | Canda, Abdullah | Cantiello, Francesco |
| Capece, Marco | Capogrosso, Paolo | Carillo, Mauro | CARLO, BUONERBA |
| Castellani, Daniele | Castiglione, Fabio | Cathcart, Paul | Cayan, Selahittin |
| Celia, Antonio | Celik, Serdar | Cellek, Selim | Challacombe, Ben |
| Chandak, Pankaj | Chandra, Ashish | Chandrasekar, Thenappan | Chang, Peter |
| Chapin, Brian | Chapple, Christopher | Chartier-Kastler, Emmanuel | Checcucci, Enrico |
| Chee, Justin | Chemasle, Christophe | Chen, Jian | Chen, Qi |
| Chen, Ronald | Chew, Ben | Chi, Thomas | Chin, Joseph |
| Chin, Peter | Chiong, Edmund | Chiriaco, Giovanni | Cho, Kang Su |
| Cho, Min Chul | Choi, Haesun | Choi, Seungtaek | Choong, Simon |
| Christopher, Andrew | Chudek, Jerzy | Chung, Jinsoo | Clark, Peter |
| Cocci, Andrea | Collins, Justin | Connell, Shea | Connolly, Stephen |
| Cook, Gary | Costello, Anthony | Cranston, David | Crawford, David |
| Cresswell, Joanne | Crestani, Alessandro | Cruz, Célia | Cruz, Francisco |
| Culig, Zoran | Cumberbatch, Marcus | Cutress, Mark | Dahm, Philipp |
| Dall’Era, Marc | Damber, Jan-Erik | Dangle, Pankaj | Danilack, V. A. |
| Danuser, Hansjoerg | Das, Akhil | DasGupta, Ranan | Davis, John |
| Davis, Niall | de Castro Abreu, Andre Luis | De La Rosette, Jean | De Luca, Stefano |
| De Nunzio, Cosimo | Del Popolo, Giulio | Delahunt, Brett | Dell’Oglio, Paolo |
| Denstedt, John | Desai, Janak | Desai, Mahesh | Deshpande, Aniruddh |
| Di Muzio, Nadia | Ding, Maylynn | Dinkelman-Smit, M. | Dizman, Nazli |
| Djordjevic, Miroslav | Dmochowski, Roger | Downing, Amy | Dragos, Laurian |
| Dudderidge, Tim | Dukic, Ivo | Dundee, Philip | Eardley, Ian |
| Eberli, Daniel | Eden, Christopher | Efstathiou, Jason | Ehdaie, Behfar |
| Eisner, Brian | El-Ghoneimi, Alaa | Elhage, Oussama | Elliott, Sean |
| Elshal, Ahmed | Elsheikh, Mohamed | Elterman, Dean | Emberton, Mark |
| Emiliani, Esteban | Engeler, Daniel | Enting, Deborah | Epstein, Jonathan |
| Erci, Behice | Everaert, Karel | Everaerts, Wouter | Fajkovic, Harun |
| Falagario, Ugo | Farhat, Walid | Ferriero, MariaConsiglia | Ferro, Matteo |
| Ficarra, Vincenzo | Figg, William | Filson, Christopher | Finch, William |
| Fiorini, Paolo | Fisch, Margit | Fisher, Rebecca | Fishman, Mayer |
| Fleshner, Neil | Fletcher, Sean | Fok, Cynthia | Fong, Eva |
| Foo, Keong Tatt | Foreman, Darren | Fraundorfer, Mark | Friberg, Anne Sofie |
| Froehner, Michael | Frydenberg, Mark | Gacci, Mauro | Gadzhiev, Nariman |
| Gakis, Georgios | Galfano, Antonio | Ghagane, Shridhar C. | Ghani, Khurshid |
| Ghose, Amit | Giannantoni, Antonella | Giannarini, Gianluca | Giganti, Francesco |
| Gild, Philipp | Gill, Inderbir | Gilling, Peter | Giusti, Guido |
| Gokce, Mehmet Ilker | Goldfarb, David | Goldman, Howard | Gontero, Paulo |
| Goossen, Hans | Gordon, Stephen | Gore, John | Gorin, Michael |
| Graefen, Markus | Gray, Elin | Greenwell, Tamsin | Gregg, Justin |
| Grey, Alistair | Grey, Benjamin | Gross, Andreas | Gross, Martin |
| Grummet, Jeremy | Gu, Meng | Gulati, Roman | Gundeti, Mohan |
| Gupta, Mohit | Gupta, Nikhil K. | Guru, Khurshid | Guruli, Georgi |
| Habous, Mohamad | Hackett, Geoff | Hadjipavlou, Marios | Hahn, Andrew |
| Hamid, Rizwan | Hamidi, Nurullah | Han, Bangmin | Han, Misop |
| Hanna, Nawar | Hanno, Philip | Hart, Nicolas | Hasan, Mudhar |
| Häuser, Lorine | Heesakkers, John | Hegarty, Paul | Heidenreich, Axel |
| Heller, Nick | Hemal, Ashok | Hennessey, Derek | Herlemann, Annika |
| Hevia, Mateo | Hindley, Richard | Hsi, Ryan S. | Huang, Jay |
| Hubscher, Charles | Huddart, Robert | Hughes, Francis | Hughes, Simon |
| Hung, Andrew | Hwang, Eu Chang | Ilg, Marcus | Ingham, Matthew |
| Irtan, Sabine | Irving, Stuart | Jack, Greg | Jeldres, Claudio |
| Jeong, Chang Wook | Jiwane, Ashish | Johnson, Mark | Joseph, Jean |
| Joshi, Pankaj | Jung, Jae Hung | Kadıoğlu, Ateş | Kahokehr, Arman |
| Kalapara, Arveen | Kalejaiye, Ayo | Kamat, Ashish | Kapoor, Jada |
| Karakiewicz, Pierre | Karam, Jose | Karunanithy, Narayan | Kasivisvanathan, Veeru |
| Kavoussi, Louis | Kaynar, Mehmet | Keeley, Frank | Kemal, Sarica |
| Khan, Azhar | Khochikar, Makarand | Khoubehi, Bijan | Kim, Isaac |
| Kim, Jae Heon | Kim, Simon | King, Martin | Kirby, Michael |
| Kirkman, Maggie | Kirsch, Andrew | Kirschner-Hermanns, Ruth | Kishan, Amar |
| Kitta, Takeya | Klaassen, Zachary | Klatte, Tobias | Knudsen, Bodo |
| Koch, Michael | Kockelbergh, Roger | Konety, Badrinath | Koo, Kevin |
| Kosaka, Takeo | Kowalczyk, Anna | Kowalewski, Tim | Krambeck, Amy |
| Krasnow, Ross | Krauss, Daniel J. | Krimphove, Marieke | Kryvenko, Oleksandr |
| Kulkarni, Ravi | Kulkarni, Sanjay | Kumar, Sunil | Kundu, Bibhas |
| Kuo, Hann-Chorng | Kusaka, M. | Kutlu, Omer | Kwon, Ohseong |
| Lam, Wayne | Lamb, Alastair | Lamb, Benjamin | Lancia, Andrea |
| Landman, Jaime | Lane, Giulia | Lange, Dirk | Laniado, Marc |
| Larcher, Alessandro | Lau, Adrian | Laudone, Vincent | Lavallée, Luke |
| Lawrenson, Ross | Lee, Byron | Lee, David | Lee, Jason Y. |
| Lee, Jongsoo | Lee, Won Ki | Lee, Young Joon | Leitner, Lorenz |
| Lerner, Lori | Lestingi, Jean | Leveridge , Michael | Levine, Larry |
| Li, Jianxing | Li, Roger | LIATSIKOS, EVANGELOS | Liauw, Stanley |
| Lieske, John | Lin, Guiting | Lingeman, James | Lipkin, Michael |
| Lipshultz, Larry | Liu, Hongbin | Løgager, Vibeke | López, Pedro José |
| Lotan, Tamara | Ma, Runzhuo | Madersbacher, Stephan | Mahal, Brandon |
| Majima, Tsuyoshi | Makanjuola, Jonathan | Malde, Sachin | Mamode, Nizam |
| Mandel, Philipp | Manecksha, Rustom | Manfredi, Matteo | Marchioni, Michele |
| Mark, Stephen | Marks, Leonard | Martin, Richard | Martinez-Salamanca, Juan |
| Martini, Alberto | Masson-Lecomte, Alexandra | Matsuda, Tadashi | Mattei, Agostino |
| Maurer, Tobias | Mayer, Erik | Mazzone, Elio | Mazzucchi, Eduardo |
| McCammon, Kurt | McClintock, Tyler | McGrath, John | McNeill, Alan |
| McNeill, S | McNicholas, Thomas | Mehan, Nicholas | Mehnert, Ulrich |
| Menichetti, Julia | Meyer, Christian | Milenkovic, Uros | Minhas, Suks |
| Mir, Maria | Misrai, Vincent | Mizokami, Atsushi | Mizuno, Kentaro |
| Modgil, Vaibhav | Modi, Parth | Modonutti, Daniele | Moncada, Ignacio |
| Monga, Manoj | Montanari, Emanuele | Montorsi, Francesco | Moochhala, Shabbir |
| Moon, Daniel | Moore, Caroline | Moran, Diarmaid | Morel Journel, Nicolas |
| MORETTI, KIM | Morey, Allen F. | Moschini, Marco | Mossanen, Matthew |
| Mostafid, Hugh | MOURMOURIS, PANAGIOTIS | Mout, Lisanne | Muir, Gordon |
| Mukhopadhyay, Subhankar | Mumtaz, Faiz | Mundy, Anthony | Muneer, Asif |
| Murphy, Adam | Murphy, Declan | Muschter, Rolf | Nabi, Junaid |
| Nair, Shiva | Najari, Bobby | Narayan, Vikram | Nathan, Senthil |
| Nazzani, Sebastiano | Netsch, Christopher | Nguyen, David-Dan | Nicolai, Nicola |
| Norberto, Bernardo | Novara, Giacomo | Nunes-Silva, Igor | O’Brien, Timothy |
| Odisho, Anobel | Ogden, Chris | Ohlander, Samuel | O’Kelly, Fardod |
| Olsburgh, Jonathon | Onem, Kadir | Osmonov, Daniar | Ost, Piet |
| Ozyavuz, Rasin | Paciotti, Marco | Pais, Jr., Vernon | Pais, Vernon |
| Pal, Sumanta | Panach-Navarrete, J. | Pang, See‑Tong | Panicker, Jalesh |
| Pannek, Jürgen | Pariser, Joseph | Patel, Hiten | Patel, Nishant |
| Patel, Prashant | Patel, Vipul | Paterson, Ryan | Patterson, Jake |
| Paul, Asit | Pavlovich, Christian | Pearce, Ian | Pearce, Shane |
| Pearle, Margaret | Penson, David | Peters, Kenneth | Pierorazio, Phillip |
| Pinsky, Paul | Pontari, Mike | Popert, Richard | Porpiglia, Francesco |
| Porten, Sima | Porter, James | Portis, Andrew | Potretzke, Aaron |
| Preminger, Glenn | Presicce, Fabrizio | Preston, Mark | Purohit, Rajveer |
| Radtke, Jan Philipp | Rai, Bhavan | Rais-Bahrami, Soroush | Raison, Nicholas |
| Ralph, David | Ramakrishnan, Venkat | Ramani, Vijay | Ramasamy, Ranjith |
| Ramaswamy, Ashwin | Ramón de Fata, Fernando | Ranasinghe, Weranja | Randhawa, Karen |
| Rane, Abhay | Rashid, Prem | Rassweiler, Jens | Rastinehad, Ardeshir |
| Ratan, Hari | Reddy, Sumeet | Rees, Geraint | Rees, Rowland |
| Reese, Stephen | Reiter, Robert | Resorlu, Berkan | Rha, Koon Ho |
| Rink, Michael | Rivera, Marcelino | Riza Kural, Ali | Robert, Grégoire |
| Roberts, Matthew | Robertson, William | Robinson, David | Rocco, Bernardo |
| Rogers, Alistair | Rogers, Craig | Roghmann, Florian | Roobol, Monique |
| Rose, Brent | Roseman, John | Ross, Ashley | Roth, Beat |
| Rottenberg, Giles | Rukin, Nicholas | Rule, Andrew | Russell, Beth |
| Russo, Giorgio Ivan | Sabnis, Ravindra | Sade, Recep | Sahai, Arun |
| Sakellariou, Christina Alexandra | Salami, Simpa | Salonia, Andrea | Salter, Carolyn |
| Samaratunga, Hemamali | Sammon, Jesse | Samnakay, Naeem | Samplaski, Mary |
| Sanchez-Salas, Rafael | Sangster, Philippa | Sarica, Kemal | Sas, David |
| Sathianathen, Niranjan | Schaeffer, Edward | Schiavina, Riccardo | Schmid, Marianne |
| Schutzer, Matthew | Sedigh, Omid | Segaran, Surayne | Seisen, Thomas |
| Sellitti, Donald | Semins, Michelle | Sengupta, Shomik | Sethia, Krishna |
| Sfakianos, John | Shao, Yi | Shaw, Greg | Shigemura, Katsumi |
| Shiranov, Kirill | Shrotri, Nitin | Shukla, Aseem | Silverman, Joshua |
| Singh, Avinash | Siva, Shankar | Skarecky, Douglas | Skolarus, Ted |
| Smith, Angela | Smith, Arthur | Smith, Thomas | Soares, Ricardo |
| Soderberg, Leah | Sodha, Hiren | Soeterik, Timo | Sofer, Mario |
| Sofikitis, Nikolaos | Sokoll, Lori | Somani, Bhaskar | Sonpavde, Guru |
| Sood, Akshay | Soomro, Naeem | Sooriakumaran, Prasanna | Speakman, Mark |
| Spiess, Phillippe | Spratt, Daniel | Srinivasan, Arun | Stai, Bethany |
| Stamatakis, Lambros | Standring, Susan | Stattin, Pär | Stebbing, Justin |
| Stephan, Carsten | Stewart, Grant | Stish, Bradley | Stoianovici, Dan |
| Stone, Nelson | Stricker, Phillip | Stroman, Luke | Studd, Rodney |
| Suardi, Nazareno | Subudhi, Sumit | Sujenthiran, Arunan | Sundi, Debasish |
| Sur, Roger | Swann, Ray | Tae, Bum Sik | Tailly, Thomas |
| Takagi, Toshio | Tan, Wei Shen | Tay, Kae Jack | Taylor, Claire |
| Te, Alexis | Teichman, Joel | Teoh, Jeremy | Tewari, Ash |
| Thalmann, George | Thimmegowda, Manohar | Thomas, Kay | Thurairaja, Ramesh |
| Tikkinen, Kari | Tilki, Derya | Torremade Barreda, Josep | Tosoian, Jeffrey |
| Tran, Maxine | Trinh, Quoc-Dien | Trinh, Vincent | Tsivian, Matvey |
| Tu, Shi-Ming | Tubaro, Andrea | Tully, Karl | Turajlic, Samra |
| Turney, Ben | Ukimura, Osamu | Urkmez, Ahmet | Uruc, Fatih |
| Uzzo, Robert | van den Bergh, Roderick | Van der Aa, Frank | Van der Kwast, Theodorus |
| Van Hemelrijck, Mieke | van Kerrebroeck, Philip | van Renterghem, Koenraad | van Rij, Simon |
| Vanni, Alex | Vasdev, Nikhil | Vasdev, Nikhil | Vela, Ian |
| Verma, Hema | Vernooij, Robin | Vicentini, Fabio C | Villers, Arnauld |
| Vivian, Justin | Wagenlehner, Florian | Wallis, Christopher | Walsh, Anna |
| Walsh, Patrick | Walton, Thomas | Wang, Shaogang | Wang, Ye |
| Ward, John | Warner, Jonathan | Watanabe, Hiroki | Watkin, Nick |
| Watson, William | Weight, Christopher | Weizer, Alon | Welk, Blayne |
| Westney, Ouida | Weston, Robin | White, Jared | Williams, Michael |
| Williams, Stephen | Willis, Susan | Winkle, David | Wiseman, Oliver |
| Withington, John | Wong, Kathie | Wong, Lih-Ming | Woo, Henry |
| Woo, Sungmin | Wood, Dan | Woon, Dixon Teck Sing | Wright, Anne |
| Wu, Wenqi | Wyant, Cole | Wysock, James | Xu, Kewei |
| Xylinas, Evanguelos | Yafi, Faysal | Yang, Dong-Rong | Yap, Tet |
| Yassaie, Omid | Yaxley, John | Ye, Dingwei | Yoshimura, Naoki |
| Zamboglou, Constantinos | Zamboni, Stefania | Zargar, Homi | Zeng, Guohua |
| Zhao, Lee | Zhu, Gang | Zhu, Xiaoye | Zondervan, Patricia |
| Zorn, Kevin |
We look forward to working with you again in 2020.
Residents’ podcast: Exercise-induced attenuation of treatment side effects in newly diagnosed PCa patients beginning androgen-deprivation therapy
Maria Uloko is a Urology Resident at the University of Minnesota Hospital. In this podcast she discusses a recent Article of the month:
Exercise‐induced attenuation of treatment side‐effects in patients with newly diagnosed prostate cancer beginning androgen‐deprivation therapy: a randomised controlled trial
Abstract
Objectives
(i) To assess whether exercise training attenuates the adverse effects of treatment in patients with newly diagnosed prostate cancer beginning androgen‐deprivation therapy (ADT), and (ii) to examine whether exercise‐induced improvements are sustained after the withdrawal of supervised exercise.
Patients and Methods
In all, 50 patients with prostate cancer scheduled for ADT were randomised to an exercise group (n = 24) or a control group (n = 26). The exercise group completed 3 months of supervised aerobic and resistance exercise training (twice a week for 60 min), followed by 3 months of self‐directed exercise. Outcomes were assessed at baseline, 3‐ and 6‐months. The primary outcome was difference in fat mass at 3‐months. Secondary outcomes included: fat‐free mass, cardiopulmonary exercise testing variables, QRISK®2 (ClinRisk Ltd, Leeds, UK) score, anthropometry, blood‐borne biomarkers, fatigue, and quality of life (QoL). HealthEd Academy can provide an extensive guides about bodybuilding, the best SARMs, Anadrole reviews and much more, take a look!
Results
At 3‐months, exercise training prevented adverse changes in peak O2 uptake (1.9 mL/kg/min, P = 0.038), ventilatory threshold (1.7 mL/kg/min, P = 0.013), O2 uptake efficiency slope (0.21, P = 0.005), and fatigue (between‐group difference in Functional Assessment of Chronic Illness Therapy‐Fatigue score of 4.5 points, P = 0.024) compared with controls. After the supervised exercise was withdrawn, the differences in cardiopulmonary fitness and fatigue were not sustained, but the exercise group showed significantly better QoL (Functional Assessment of Cancer Therapy‐Prostate difference of 8.5 points, P = 0.034) and a reduced QRISK2 score (−2.9%, P = 0.041) compared to controls.
Conclusion
A short‐term programme of supervised exercise in patients with prostate cancer beginning ADT results in sustained improvements in QoL and cardiovascular events risk profile.
BJUI Podcasts are available on iTunes: https://itunes.apple.com/gb/podcast/bju-international/id1309570262