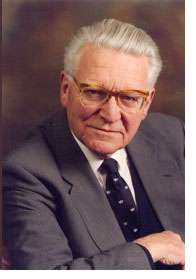
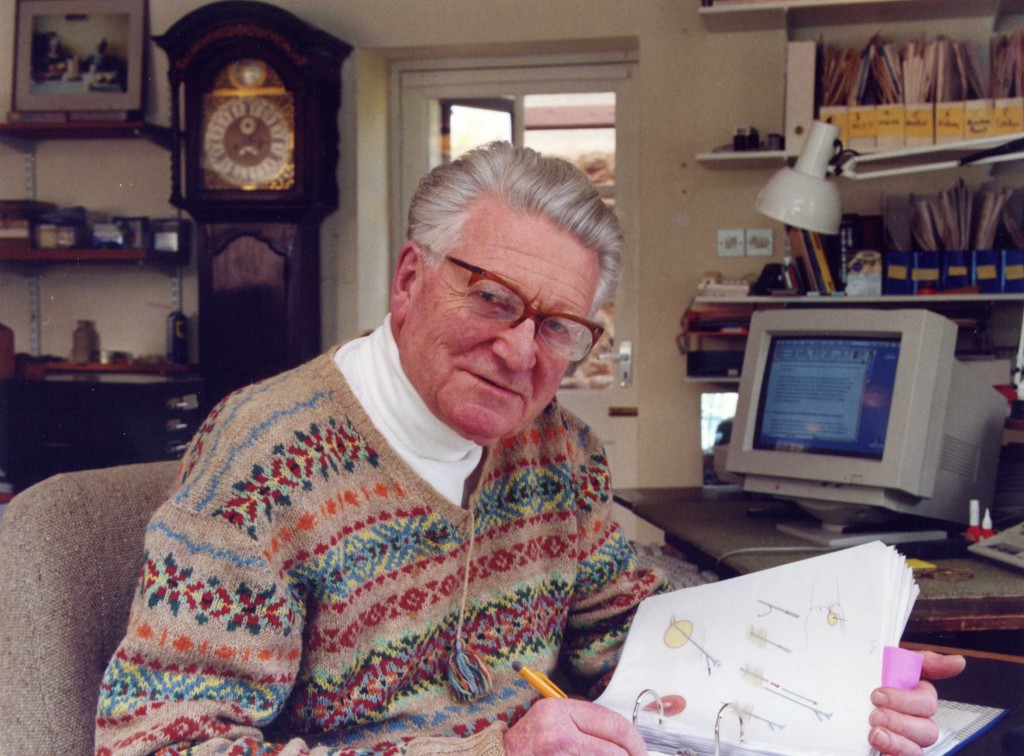
Richard Turner-Warwick
Richard Turner-Warwick CBE MSc, MCh (Oxon), DM.(Oxon), DSc.(Hon NY), FRCP, FRCS, FRCOG, FACS, FRACS (Hon), FACS (Hon)
Richard Turner-Warwick, now retired, but in good health, was one of the giants of British urology and is, quite literally, the Father of reconstructive urology, both nationally and internationally. A brilliant surgeon, teacher and writer, he managed to inspire a great many urologists around the world. He also restored quality of life to countless patients from many continents who had suffered traumatic or neoplastic injury to their genitals or lower urinary tract. In his honour we have organized a meeting on reconstructive urology, kindly supported by The Urology Foundation (TUF), in Glasgow on Saturday 12th October 2014, immediately in advance of the SIU meeting in the same city. This blog is designed to publicise this meeting, and also provide an opportunity for those that worked with and for Richard to post their memories and reminiscences of the great man. Please do post a comment, and also join us in Glasgow at what will certainly be an exceptional day.
LINK TO REGISTER: https://tinyurl.com/RTWmeeting
Biography
 Born in 1925, Richard Turner-Warwick was educated at Bedales School – at Oxford University and at The Middlesex Hospital Medical School in London. At Oxford he took an honours degree in Natural Science.
Born in 1925, Richard Turner-Warwick was educated at Bedales School – at Oxford University and at The Middlesex Hospital Medical School in London. At Oxford he took an honours degree in Natural Science.
He was captain of the Oriel College Boat Club, rowed in the 1944, 1945 Oxford Crews and won the Oxford and Cambridge Boat Race in 1946 when he was President of the OUBC. His MSc thesis was on Neuro-Anatomy.
During his pre-clinical training at The Middlesex Hospital he obtained the Senior Broderip Scholarship and a number of other Medals and Prizes – qualifying in 1949. From 1949 until 1960, mostly at The Middlesex Hospital, he had an unusually extensive specialist training in internal medicine and pathology – and then in abdominal, thoracic, gynecological, and plastic surgery. He trained in urological surgery with Sir Eric Riches and with Sir David Innes Williams at the Institute of Urology in London.
He obtained his FRCS in 1954, his MRCP in 1955, his Oxford Doctorate of Medicine in 1957 and his Oxford Mastership of Surgery in 1962. He was able to visit many urological centres in America as the Comyns Berkley Travelling Fellow – becoming a Senior Resident in Urology at the Columbia-Presbyterian Medical Centre in New York. He was appointed a Consultant General Surgeon to The Middlesex Hospital in 1960 – one of six, with additional charge of the Thyroid Clinic. His outpatient assistant at this time was Deborah Doniach, the pioneer of clinical auto-immunity – her treatment of Hashimoto’s lymphadenoid goitre with thyroxine led to its shrinkage so that decompression-thyroidectomy no longer provided the control histological material she needed – it was for this purpose that he developed his trephine biopsy instrument.
He took over the Urological Department at The Middlesex Hospital when Sir Eric retired in 1963. He created a pioneering urodynamic unit as an integral part of his routine clinical service – synchonously combining video-cysto-urethrography with measurement of pressure and flow voiding dynamics.
Since about 1975 he confined his personal surgical interest and practise to Functional Reconstruction – he was additionally appointed to the staff of St Peter’s Urological Hospitals in London and also an Honorary Visiting Urological Surgeon to the Royal Prince Alfred Hospital in Sydney in 1978 where he operated for three weeks each year until 1987. His main interest and reputation at that time was in reconstruction of the male urethra.
 He was elected a Hunterian Professor of the Royal College of Surgeons in 1977, later serving on the Council of this and also that of the Royal College of Obstetricians and Gynaecologists. He was President of the British Association of Urological Surgeons 1982-1984. Among his many distinctions he was given the Victor Bonney prize of the RCOG; in 1987, the Valentine Gold Medal of the New York Academy of Medicine in 1991, the Gordon Watson Medal of the RCS in 1992, the Spence Medal of the American Association of Genito-Urinary Surgeons in 1997 and the William Didusch award of the for medical art in 2002.
He was elected a Hunterian Professor of the Royal College of Surgeons in 1977, later serving on the Council of this and also that of the Royal College of Obstetricians and Gynaecologists. He was President of the British Association of Urological Surgeons 1982-1984. Among his many distinctions he was given the Victor Bonney prize of the RCOG; in 1987, the Valentine Gold Medal of the New York Academy of Medicine in 1991, the Gordon Watson Medal of the RCS in 1992, the Spence Medal of the American Association of Genito-Urinary Surgeons in 1997 and the William Didusch award of the for medical art in 2002.
He was elected to FACS (Hon). in 1997, to FRACS (Hon) in 1981, to elite Fellowship of the Urological Society of Australia in 1988 the Honorary Fellowship of the American Association of Genito-Urinary Surgeons in 2002. He was awarded an Honorary Doctorate of Science in New York in 1988. During the 40 years between 1965 and 2005 he undertook more than 300 operating surgical teaching visits – mostly in America, Australia, New Zealand but also in Europe and the UK.
The Genesis of Urethral Reconstructive Surgery over the Last 50 Years
In Honour of Richard Turner-Warwick
Friday 10th – Saturday 11th October 2014
Royal College of Physicians and Surgeons, Glasgow
LINK TO REGISTER: https://tinyurl.com/RTWmeeting
Friday 10th October
Afternoon Arrival
19:00 Dinner – with reflections by attendees
Royal College of Surgeons & Physicians, Glasgow
Saturday 11th October
09:00 Welcome and Introduction
Christopher Chapple & Roger Kirby
09.05 A Lifetime’s Experience of Urethral Surgery
Richard Turner-Warwick
09:15 Genesis of Anterior Urethral Surgery: From Scrotum to Oral Mucosa
Jack McAninch
(15 minutes talk, with 5 minutes questions and discussion)
09:35 Developments in Bladder Reconstruction
Anthony Stone
(15 minutes talk, with 5 minutes questions and discussion)
09:55 Anastomotic Urethroplasty: To Transect The Urethra Or Not? The Heineke Mikulicz Approach
Julian Shah
(15 minutes talk, with 5 minutes questions and discussion)
10:15 Oral Mucosa and Beyond
Richard Inman
(15 minutes talk, with 5 minutes questions and discussion)
10:35 Effective Management of Lichen Sclerosis
Sanjay Kulkarni
(15 minutes talk, with 5 minutes questions and discussion)
10:55 Break for Morning Coffee
11:15 Reflections on a Lifetime’s Practice
James Wong
(15 minutes talk, with 5 minutes questions and discussion)
11:35 Lessons Learned From the Use of Stents
Christopher Chapple
(15 minutes talk, with 5 minutes questions and discussion)
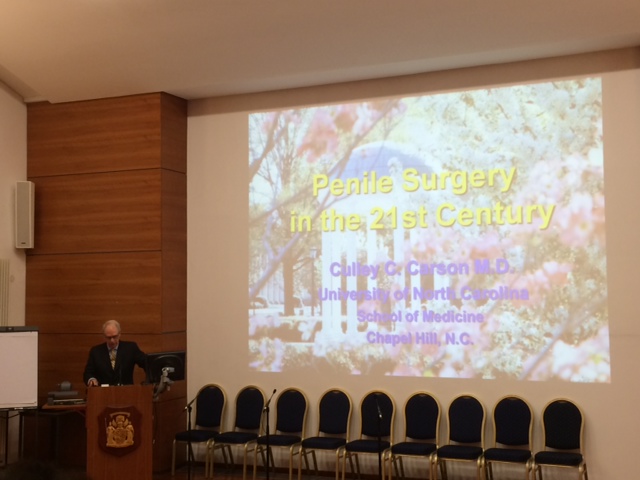
11:55 Penile Surgery
Culley Carson
(15 minutes talk, with 5 minutes questions and discussion)
12:15 Hypospadias
Patrick Duffy
(15 minutes talk, with 5 minutes questions and discussion)
12:35 Break for Lunch
13:30 Difficult Retrieval Surgery
Tony Mundy
(15 minutes talk, with 5 minutes questions and discussion)
13:50 Colonic Mucosal Graft Ventral Onlays Utilizing the TEM Transanal Approach
Leonard Zinman
(15 minutes talk, with 5 minutes questions and discussion)
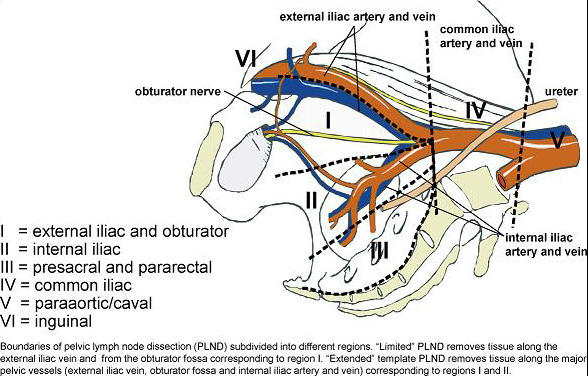
14:10 Development of Contemporary Management of Pelvic Fracture Urethral Distraction Injury
George Webster
(15 minutes talk, with 5 minutes questions and discussion)
14:30 Posterior Urethral Reconstruction Following Radical Prostate Surgery: Minimally Invasive Approaches to the Posterior Urethra
Roger Kirby
(15 minutes talk, with 5 minutes questions and discussion)
14:50 Round Table Discussion
All speakers
What do we do well? What don’t we do so well? What needs to be developed for the future? Who should carry out surgery? How should they be trained? Is there a minimum number of procedures somebody should do per year? How should we assess outcomes? (45 minutes)
15:35 Summary of meeting (10 minutes)
15:45 Meeting Closes