We live in a dehumanizing world. Out of a need for efficiency, convenience, and reassurance, we both dehumanize and are dehumanized routinely in our commerce and relationships. We are not a three-dimensional human being of unique genetics and experience, forte and frailty, preferences and peculiarities to our bank, public library, or insurance company. Out of necessity, these structures diminish us to a number or barcode. We are grouped by age and demographic, measured by our internet clicks, targeted according to our income by corporations. To those profiting from our consumption our individuality is irrelevant; the big money is in exploiting groups. Whether you support a free Tibet does not concern the people selling cheeseburgers, unless enough people agree with you that some marketing leverage can be generated from this fact. In medical research we reduce people to “female between 40 and 75 years with chemotherapy naïve metastatic ovarian carcinoma”. Not “Julie, mother of three boys (one with cerebral palsy), who put up with her vague abdominal symptoms for too long because she was preoccupied by supporting her younger sister out of an abusive relationship”. While logistical limitations do not allow for the statisticians to enter into every individual story, we reassure ourselves that the depersonalized and homogenized data from these studies is for the greater good. Indeed, sometimes it just isn’t any of our business.
We live in a dehumanizing world. Out of a need for efficiency, convenience, and reassurance, we both dehumanize and are dehumanized routinely in our commerce and relationships. We are not a three-dimensional human being of unique genetics and experience, forte and frailty, preferences and peculiarities to our bank, public library, or insurance company. Out of necessity, these structures diminish us to a number or barcode. We are grouped by age and demographic, measured by our internet clicks, targeted according to our income by corporations. To those profiting from our consumption our individuality is irrelevant; the big money is in exploiting groups. Whether you support a free Tibet does not concern the people selling cheeseburgers, unless enough people agree with you that some marketing leverage can be generated from this fact. In medical research we reduce people to “female between 40 and 75 years with chemotherapy naïve metastatic ovarian carcinoma”. Not “Julie, mother of three boys (one with cerebral palsy), who put up with her vague abdominal symptoms for too long because she was preoccupied by supporting her younger sister out of an abusive relationship”. While logistical limitations do not allow for the statisticians to enter into every individual story, we reassure ourselves that the depersonalized and homogenized data from these studies is for the greater good. Indeed, sometimes it just isn’t any of our business.
We can accept that on this macro level there are faceless amoral corporations that care only about how to alter our spending patterns, but on an interpersonal level we can be equally guilty of dehumanizing attitudes. Thanks to the heuristics developed by our ancestors, which I for one am grateful for, the human brain is very efficient at mentally grouping things under such headings as “dangerous” and “delicious”. This has allowed our continued survival. Having a general suspicion of things that looks like snakes means a reduced risk of envenomation. Being suspicious of strangers by default means that we are less likely to be on the back foot if someone pulls a spear on us. It would be nice to think that we have largely put this simplistic cognitive process behind us, but we tend to fall back on bad habits. Every time we mentally label a person we are trimming their humanity in order to fit them into a pre-existing cognitive category. When we think “young hoodlum”, “old codger”, “drug addict”, “liberal”, or “health nut”, we are in fact extracting what we deem to be the most salient point of person and making it the sum total of their identity. There is obviously expedient for us, as we continue to do it. It makes it easier to ignore the “derelict” on the street, and not feel too bad about the “foreigners” affected by natural disasters. Our bias is routinely exploited by our leaders, especially in times of war. We are not killing people very similar to ourselves, we are fighting “scum”, “heretics”, “commies”. While studying for a degree in psychology I came across a study that demonstrated that people attribute more negative characteristics to people groups if they are referred to by nouns rather than adjectives. People were more mistrustful of others described as “Poles” or “Jews”, rather than “Polish” or “Jewish”. The objective label nudges people into a category, with the adjective reminds us that these are complex individuals, who happen to have a given ethnicity or faith.
We have a reflexive discomfort at being dehumanized ourselves. We don’t like being treated like cattle by airlines or sports stadiums. We despise being written off as nothing more than the town we came from, the school we went to, the era we grew up in, or our gender. We know from personal experience that we are unique, and attribute value to this, at least in ourselves.
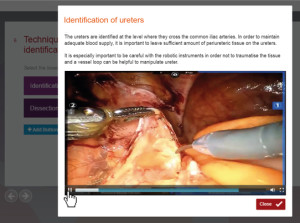
Surgery is dehumanizing. We take frightened people, anaesthetize them so that they cannot resist, and then disassemble them. The intention is to reassemble them in an improved way, but we are reducing people to a collection of organs and meat in a way that strips them of usual dignity. Until the Renaissance, disassembling the dead was considered too shameful to tolerate. Indeed, to begin with only executed criminals, considered sub-human (already dehumanized), were considered suitable candidates for anatomical dissection. It was too much to imagine a person opened up for the world to see their insides, their dignity stripped in an extreme form of nudity. I have already written about how not entering into the full experience of every human drama is what makes surgery a viable career (https://www.bjuinternational.com/bjui-blog/surgery-is-not-normal/), and I don’t think it is helpful to focus on the bigger picture beyond the operating theatre while focusing on the technical steps of an operation, but a few points are worth considering.
Firstly, those of us who have had human dissection as a part of our training tend to share a common experience. While in the thick of a dissection, occasionally rewarded with the discovery of a familiar structure, it is normal to forget that the prosection was once the residence of a functioning person. Typically it is the glimpse of a uniquely human feature; the face, feet, hands that triggers a moment of shock at what is going on. I still recall looking down to see that our cadaver had painted toenails. Instead of being a learning resource, it struck me that this woman had spent time days before her death, tending to her toenails fastidiously, unaware of what was to come. This placed her in a room in her home, at a time of day, perhaps before leaving to attend a social event. The full experience of her humanity was infinitely greater than the tutorial aid she had been reduced to. The strict procedures governing the use of human tissue made sense, lest we forget the gift of the donor.
One of the more moving experiences I have had in a hospital is watching Intensive Care nurses managing comatose patients. My observation is that these patients are treated more gently than necessary, and there is a constant one-way conversation from the nurses explaining that now, they are going to reposition the legs. They are going to brush teeth. They are adjusting the pillow. Calling the patient by their name, as their words fall on deaf ears. While logically this makes no difference to medical treatment, it protects the nurse from dehumanizing the patient, making them more than an oxygen trace on a screen.
Ultimately, the effort to re-humanize is what makes us fully human. The unconscious patient or cadaver is not affected by our attitude towards them, but we sacrifice our own humanity whenever we revert to applying broad heuristics to other people. A cat knows to be frightened of snakes, but it takes human intelligence and will to deliberately consider that a person is more than something to fear, ignore, or desire. It is an act of overcoming base instinct. When we apply the appropriate reverence for a person as we prepare them for surgery, care for them in their unconsciousness, our respectfully use their dead body to improve the treatment of future patients, we affirm our own humanity. It is more for us than for them.
Jim Duthie is a Urological Surgeon/Robotic Surgeon. Interested in Human Factors Engineering, training & error, and making people better through electronic means. Tauranga, New Zealand. @Jamesduthie1
 Most of the authors of this issue’s Article of the Month work in Zurich, Switzerland. The cover image shows the Sphinx Observatory, one of the highest astronomical observatories in the world, at Jungfraujoch in the Swiss Alps.
Most of the authors of this issue’s Article of the Month work in Zurich, Switzerland. The cover image shows the Sphinx Observatory, one of the highest astronomical observatories in the world, at Jungfraujoch in the Swiss Alps.