Introducing The Urology Green List
 The world of predatory scientific publishing had a major ‘win’ when Jeffrey Beall’s blog “Scholarly Open Access” was suddenly emptied of content in January 2017. Beall was tireless in his attempts to expose the unscrupulous behaviour of predatory open access journals whose objective was nothing other than to extract author publication charges (APCs) from unwitting academics. His blog was very much the “go to” site if one wished to check the legitimacy of a particular open access journal. In a confusing publishing landscape, it was an essential guidance on which open access journals were to be avoided. The growth of this predatory publishing industry has been exponential and clearly a reflection of the enormous amount money that is there to be made. Beall was constantly under attack from predatory publishers including threats of litigation. Beall has gone to ground and this normally vocal bastion of transparency has provided no reason for the sudden deletion of content from the Scholarly Open Access blog.
The world of predatory scientific publishing had a major ‘win’ when Jeffrey Beall’s blog “Scholarly Open Access” was suddenly emptied of content in January 2017. Beall was tireless in his attempts to expose the unscrupulous behaviour of predatory open access journals whose objective was nothing other than to extract author publication charges (APCs) from unwitting academics. His blog was very much the “go to” site if one wished to check the legitimacy of a particular open access journal. In a confusing publishing landscape, it was an essential guidance on which open access journals were to be avoided. The growth of this predatory publishing industry has been exponential and clearly a reflection of the enormous amount money that is there to be made. Beall was constantly under attack from predatory publishers including threats of litigation. Beall has gone to ground and this normally vocal bastion of transparency has provided no reason for the sudden deletion of content from the Scholarly Open Access blog.
You can’t help to ask the following questions about the predatory publishing industry. How do these journals make such inroads into academia? How do they manage to outwit highly intelligent individuals to support their journal either through the submission of manuscripts or editorial board duties? The answer is quite simple. They prey on the naivety, vulnerability and egos of academics.
Spam email casts a wide net. Cast it wide enough and somebody is bound to get caught. The standards required to publish articles in good journals has never been so high and the pressure to publish weighs heavy in the minds of academics. These emails will always find an email inbox of a researcher on the rebound after the rejection of a manuscript from a reputable journal. The language of the emails use flattery and an expert sales pitch to appeal to the recipient into submitting an article and then later discovering excessive APCs. If payment is refused, the article is published in any case; as a result of this action, they are deprived of the opportunity to submit their work elsewhere.
The same language is used to appeal to urologists to become members of editorial boards. Those accepting these roles unwittingly allow these journals to trade on their good name as well as the good name of their institutions to prop up their otherwise shonky image. These academics inadvertently contribute to the flow of manuscripts to these journals as a result of researchers associating the credibility of editorial board members with the credibility of the journal.
Beall’s focus was very much on where not to publish. The recent events suggest that a change in direction is needed. Accordingly, the Urology Green List has been created. The focus is all about good journals, both subscription and open access, where it is considered safe for the urological community to send their research for publication. Beall demonstrated that it was a never ending task trying to keep up with an exponential growth in the numbers of predatory journals. It is far more practical to maintain a list of journals where it is safe to publish.
Absence from the list does not mean that a journal must be avoided – absence is nothing more than a red flag suggesting that there be appropriate due diligence in establishing the authenticity of the journal and to ask colleagues, friends and mentors for advice.
The Urology Green List will be a living on line document. Visitors will be encouraged to make suggestions on which journals should be added to the list and which journals should be removed from the list. In the near future, an International Editorial Board will be established to assist with providing opinion and review of journals that are for inclusion or exclusion from the Urology Green List.
In the longer term, a project will be to develop objective criteria for which journals on the Urology Green List may be assessed and graded. In the future, it is hoped that researchers can be provided with guidance to understand the ‘best fit’ venue for their research amongst the journals that reside on the Urology Green List.
Please come and visit the Urology Green List. It is here to support the urological community. Feedback is always welcome.
https://urologygreenlist.wordpress.com/
________________________
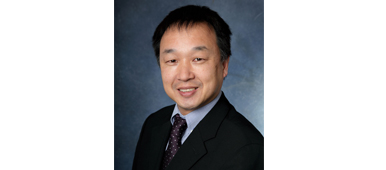
Henry Woo is a urological surgeon. He is Professor of Surgery (Urology) at the Sydney Adventist Hospital Clinical School of the University of Sydney. He is also the Director of Uro-Oncology and Professor of Robotic Cancer Surgery at the Chris O’Brien Lifehouse cancer service in Sydney. @drhwoo