Editorial: Radical cystectomy: how do blood transfusions affect oncological outcomes?
Kluth et al. [1] have conducted a large retrospective study from several institutions in North America and Europe to assess the impact of blood transfusion on oncological outcomes after radical cystectomy (RC) for bladder cancer. The hypothesis for a negative impact of transfusion on oncological outcomes stems from the observation that renal allograft survival is prolonged after pre-transplant blood transfusions because of its immuno-modulatory effects [2]. This finding prompted Gantt [3] to express concern about the possible adverse effects of transfusions in patients being treated for cancer. Since then, there have been numerous publications addressing this issue in various surgical journals including those of urology with conflicting messages.
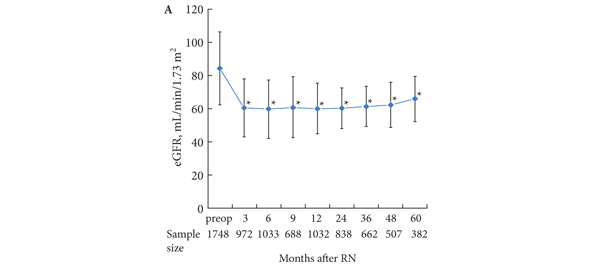
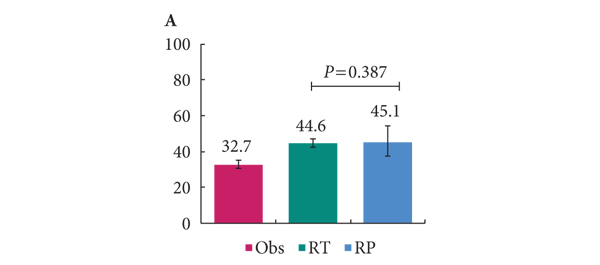
Sadeghi et al. [4] queried the Columbia University Urologic Oncology Database. This included 638 patients undergoing RC between 1989 and 2010. Of these, 209 (32.8%) received perioperative blood transfusions. On univariate analysis, the number of units transfused was inversely related to overall and cancer-specific survival. However, on multivariate analysis, it did not prove to be an independent predictor of cancer-specific survival.
As the authors highlighted in this paper, Linder et al. [5] reported a large series of patients from the Mayo Clinic, which included 2060 patients undergoing RC over 25 years. Of this large cohort, 1279 (62%) received perioperative blood transfusion with adverse outcomes, not only in terms of overall and cancer-specific mortality, but also postoperative tumour recurrence.
RC is one of the most major surgical procedures performed in urological surgery. The vast majority of patients with bladder cancer requiring RC are in their mid-sixties, overweight and have several co-morbidities. Some of these patients present late and are anaemic at presentation.
Blood loss during open RC varies depending upon surgeons’ experience, patients’ body mass index, disease stage and availability of modern equipment, e.g. LigaSure™ or stapling devices. Blood transfusion may be required because of pre-existing anaemia or excessive blood loss during surgery. Variations exist in thresholds of anaesthesiologists and the surgeons for transfusions. All of these factors account for variation in reported frequency of transfusion rates for this operation and this is well reflected in many large series of RC.
As there are many confounding factors that may influence overall and cancer-specific survival in patients undergoing RC including stage of the disease, histological nature of the tumour, lymph node status and competing co-morbidities, it is very challenging to control for these factors in retrospective series. Hence, prospective well-controlled multicentre studies are the only way forward to answer this question.
While we await robust evidence on the influence of perioperative transfusion on oncological outcomes, several potential options could be explored to avoid homologous blood transfusion. These include preoperative optimisation of haemoglobin levels through iron infusions, administration of erythropoietin where appropriate, and preoperative autologous-banking. Intraoperatively meticulous surgical technique, use of modern devices, e.g. LigaSure/stapler and Cell Savers, could be used to avoid homologous blood transfusion.
Fortunately, these studies aimed at raising awareness of potential risks of transfusions are appearing in the urological literature at a time when urologists are moving away from open to minimally invasive oncological surgery with a steady decline in the need for perioperative blood transfusion. This is one of the important steps in the right direction and will have a major impact on the need for blood transfusion in foreseeable future.
Muhammed S. Khan
Department of Urology, Guy’s Hospital and King’s College London School of Medicine, London, UK
References
- Kluth LA, Xylinas E, Rieken M et al. Impact of perioperative blood transfusion on the outcome of patients undergoing radical cystectomy for urothelial carcinoma of the bladder. BJU Int 2014; 113: 393–398
- Opelz G, Sengar DP, Mickey MR, Terasaki PI. Effect of blood transfusions on subsequent kidney transplants. Transplant Proc 1973; 5: 253–259
- Gantt CL. Red blood cells for cancer patients. Lancet 1981; 2: 363
- Sadeghi N, Badalato GM, Hruby G, Kates M, McKiernan JM. The impact of perioperative blood transfusion on survival following radical cystectomy for urothelial carcinoma. Can J Urol 2012; 19: 6443–6449
- Linder BJ, Frank I, Cheville JC et al. The impact of perioperative blood transfusion on cancer recurrence and survival following radical cystectomy. Eur Urol 2013; 63: 839–845