Video: Prostatic urethral lift for the treatment of LUTS
Multicentre prospective crossover study of the ‘prostatic urethral lift’ for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia
Anthony L. Cantwell, William K. Bogache*, Steven F. Richardson†, Ronald F. Tutrone‡, Jack Barkin§, James E. Fagelson¶, Peter T. Chin†† and Henry H. Woo
‡‡Atlantic Urological Associates, Daytona Beach, FL, *Carolina Urological Research Center, Myrtle Beach, SC, †Western Urological Clinic, Salt Lake City, UT, ‡Chesapeake Urology, Baltimore, MD, USA, §University of Toronto, Toronto, ON, Canada, ¶Urology Associates of Denver, Denver, CO, USA, ††Figtree Private Hospital, Figtree, and ‡‡Sydney Adventist Hospital Clinical School, University of Sydney, Sydney, NSW, Australia
OBJECTIVE
• To assess the clinical effect of the ‘prostatic urethral lift’ (PUL) on lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH) through a crossover design study.
PATIENTS AND METHODS
• Men aged ≥50 years with an International Prostate Symptom Score of ≥13, a maximum urinary flow rate (Qmax) of ≤12 mL/s, and a prostate of 30–80 mL were enrolled into a crossover study after completing a prospective, randomised, controlled, ‘blinded’ pivotal study in which they were control subjects receiving a sham procedure.
• Patients were followed for 1 year after crossover PUL at 19 centres in the USA, Canada and Australia. The sham procedure involved rigid cystoscopy with simulated active treatment sounds.
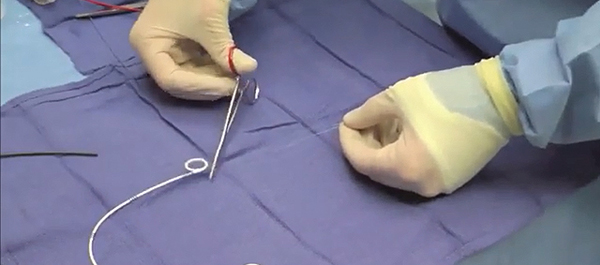
• PUL involved placing permanent UroLift® (NeoTract, Inc., Pleasanton, CA, USA) implants into the lateral lobes of the prostate to enlarge the urethral lumen.
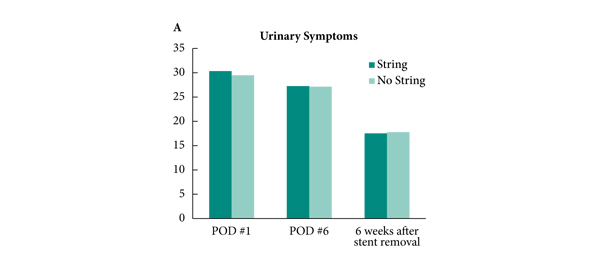
• Urinary symptom relief, health-related quality of life (HRQL) impact, urinary flow parameters, sexual function, and adverse events were assessed and compared between the sham and PUL using paired statistical analysis.
RESULTS
• Symptom, flow, HRQL and sexual function assessments showed response improvements from baseline results, similar to results from other published studies, and most parameters were markedly improved after PUL vs the sham procedure in the same patients.
• Symptom, flow, and HRQL improvements were durable over the 12 months of the study.
• Adverse events associated with the procedure were typically transient and mild to moderate; one patient (2%) required re-intervention with transurethral resection of the prostate in the first year.
• There were no occurrences of de novo, sustained ejaculatory or erectile dysfunction.
CONCLUSION
• The PUL can be performed under local anaesthesia, causes minimal associated perioperative complications, allows patients to quickly return to normal activity, provides rapid and durable improvement in symptoms, and preserves sexual function.