Article of the week: Outcomes of PCNL in England
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
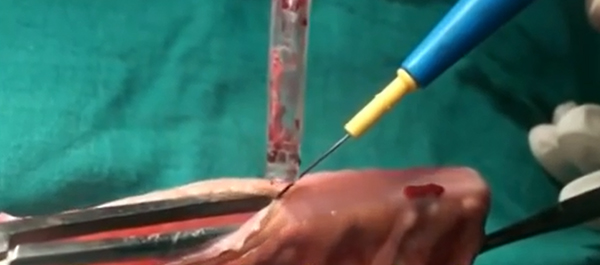
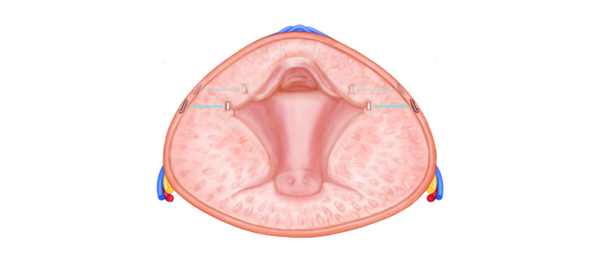
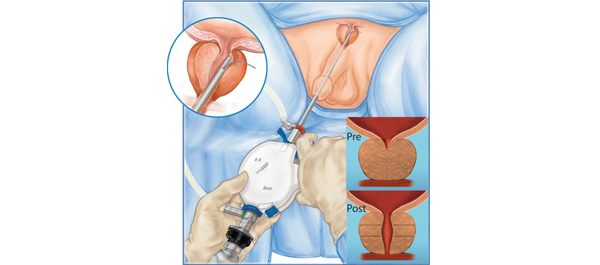
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Mr. Armitage and Mr. Withington discussing their article.
If you only have time to read one article this week, it should be this one
Percutaneous nephrolithotomy in England: practice and outcomes described in the Hospital Episode Statistics database
James N. Armitage, John Withington*†, Jan van der Meulen*‡, David A. Cromwell*, Jonathan Glass†, William G. Finch§, Stuart O. Irving§ and Neil A. Burgess§
Department of Urology, Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge, *Clinical Effectiveness Unit, The Royal College of Surgeons of England, †Department of Urology, Guy’s & St Thomas’ NHS Foundation Trust, ‡London School of Hygiene and Tropical Medicine, London, and §Department of Urology, Norfolk and Norwich University Hospitals NHS Foundation Trust, Norwich, UK
OBJECTIVE
• To investigate the postoperative outcomes of percutaneous nephrolithotomy (PCNL) in English National Health Service (NHS) hospitals.
PATIENTS AND METHODS
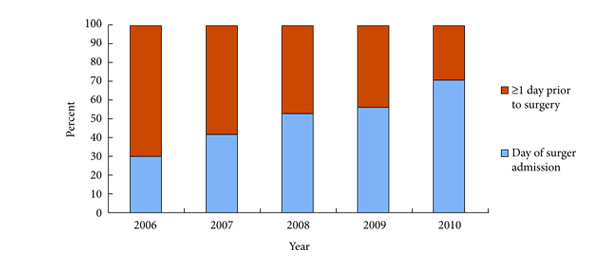
• We extracted records from the Hospital Episode Statistics (HES) database for all patients undergoing PCNL between March 2006 and January 2011 in English NHS hospitals.
• Outcome measures were haemorrhage, infection within the index admission, and rates of emergency readmission and in-hospital mortality within 30 days of surgery.
RESULTS
• A total of 5750 index PCNL procedures were performed in 165 hospitals.
• During the index admission, haemorrhage was recorded in 81 patients (1.4%), 192 patients (3.8%) had a urinary tract infection (UTI), 95 patients (1.7%) had fever, and 41 patients (0.7%) had sepsis.
• There were 595 emergency readmissions in 518 patients (9.0%). Reasons for readmission were varied: 70 (1.2%) with UTI, 15 (0.3%) sepsis, 73 (1.3%) haematuria, 25 (0.4%) haemorrhage, and 25 (0.4%) acute urinary retention.
• There were 13 (0.2%) in-hospital deaths within 30 days of surgery.
CONCLUSIONS
• Haemorrhage and infection represent relatively common and potentially severe complications of PCNL.
• Mortality is extremely rare after PCNL (about one in 400 procedures overall) but almost one in 10 patients have an unplanned hospital readmission within 30 days of surgery.
• Complications of PCNL may be under-reported in the HES database and need to be corroborated using other data sources.