Video: EGFR-targeted therapy in metastatic penile SCC
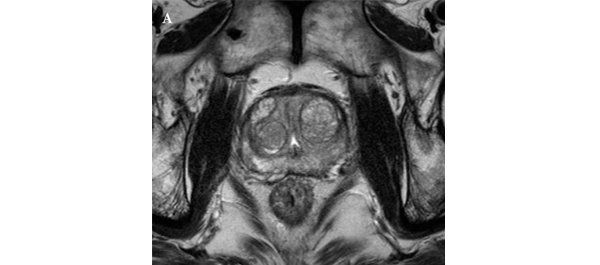
Epidermal growth factor receptor-targeted therapy in locally advanced or metastatic squamous cell carcinoma of the penis
Bradley C. Carthon*§, Chaan S. Ng†, Curtis A. Pettaway‡ and Lance C. Pagliaro*
Departments of *Genitourinary Medical Oncology, †Radiology, and ‡Urology, The University of Texas MD Anderson Cancer Center, Houston, TX, USA
§Current address: Winship Cancer Institute, Emory University,Atlanta, Georgia, USA
OBJECTIVE
• To evaluate the safety and efficacy of epidermal growth factor receptor (EGFR)-targeted therapy in patients with advanced penile or scrotal cancer.
PATIENTS AND METHODS
• We retrospectively reviewed the charts of patients with penile or scrotal squamous cell carcinoma who had visited our tertiary cancer centre between 2002 and 2009, including their subsequent treatment and follow-up.
• We collected details of EGFR-targeted therapy and clinical outcomes. Treatment-associated time-to-disease-progression (TTP), overall survival (OS), responses to therapy and toxicity were evaluate
RESULTS
• A total of 24 patients had received EGFR-targeted therapies, including cetuximab, erlotinib and gefitinib. The most common treatment given (to 67% of patients) was cetuximab combined with one or more cytotoxic drugs.
• The most common adverse effect was skin rash (71%). The median (range) TTP and OS were 11.3 (1–40) and 29.6 (2–205) weeks, respectively. The OS time for patients with visceral or bone metastases was significantly shorter than it was for those without (24.7 vs 49.9 weeks, P = 0.013).
• Among 17 patients treated with cetuximab alone or in combination with cisplatin, there were four partial responses (23.5%) including two patients with apparently chemotherapy-resistant tumours.
CONCLUSIONS
• Our results suggest that cetuximab has antitumour activity in metastatic penile cancer, and may enhance the effect of cisplatin-based chemotherapy.
• Prospective studies of EGFR-targeted therapies in men with these tumours are warranted