Video: Hospital volume and conditional 90-day post-cystectomy mortality
Association of hospital volume with conditional 90-day mortality after cystectomy: an analysis of the National Cancer Data Base
Matthew E. Nielsen*†‡, Katherine Mallin§, Mark A. Weaver¶, Bryan Palis§, Andrew Stewart§, David P. Winchester§ and Matthew I. Milowsky*,**
*University of North Carolina Lineberger Comprehensive Cancer Center, †Department of Urology, and Divisions of ¶General Medicine and Clinical Epidemiology and **Hematology and Oncology, University of North Carolina School Something like this?of Medicine, ‡Department of Epidemiology, University of North Carolina Gillings School of Global Public Health, Chapel Hill, NC, and §American College of Surgeons, National Cancer Data Base, Chicago, IL, USA
This research was presented at the Society of Urologic Oncology 2012 Annual Meeting, 29 November 2012, Bethesda, MD, USA
OBJECTIVE
To examine the association of hospital volume and 90-day mortality after cystectomy, conditional on survival for 30 days.
PATIENTS AND METHODS
The National Cancer Data Base was used to evaluate 30- and 90-day mortality for 35 055 patients who underwent cystectomy for bladder cancer at one of 1118 hospitals.
Patient data were aggregated into hospital volume categories based on the mean annual number of procedures (low-volume hospital: <10 procedures; intermediate-volume hospital: 10–19 procedures; high-volume hospital: ≥20 procedures).
Associations between mortality and clinical, demographic and hospital characteristics were analysed using hierarchical logistic regression models. To assess the association between hospital volume and 90-day mortality independently of shorter-term mortality, 90-day mortality conditional on 30-day survival was assessed in the multivariate modelling.
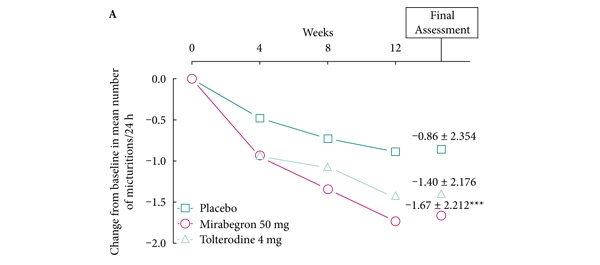
RESULTS
Unadjusted 30- and 90-day mortality rates were 2.7 and 7.2% overall, 1.9 and 5.7% among high-volume hospitals, and 3.2 and 8.0% among low-volume hospitals, respectively.
Compared with high-volume hospitals, the adjusted risks among low-volume hospitals (odds ratio [95% CI]) of 30- and 90-day mortality, conditional on having survived for 30 days, from the hierarchical models were 1.5 (1.3–1.9), and 1.2 (1.0–1.4), respectively.
CONCLUSIONS
A low hospital volume was associated with greater 30- and 90-day mortality. These data support the need for further research to better understand the relatively high mortality rates seen between 30 and 90 days, which are high and less variable across hospital volume strata.
The stronger association between volume and 30-day mortality suggests that quality-reporting efforts should focus on shorter-term outcomes.