Video: Prognostic value of neutrophil–lymphocyte ratio in patients with UTUC
Validation of pretreatment neutrophil–lymphocyte ratio as a prognostic factor in a European cohort of patients with upper tract urothelial carcinoma
Orietta Dalpiaz, Georg C. Ehrlich, Sebastian Mannweiler*, Jessica M. Martín Hernández, Armin Gerger†, Tatjana Stojakovic‡, Karl Pummer, Richard Zigeuner, Martin Pichler† and Georg C. Hutterer
Department of Urology, *Institute of Pathology, †Division of Oncology, Department of Internal Medicine, and ‡Clinical Institute of Medical and Chemical Laboratory Diagnostics, Medical University of Graz, Graz, Austria
OBJECTIVE
• To investigate the potential prognostic significance of the neutrophil–lymphocyte ratio (NLR) in a large European cohort of patients with upper urinary tract urothelial cell carcinoma (UUT-UCC).
PATIENTS AND METHODS
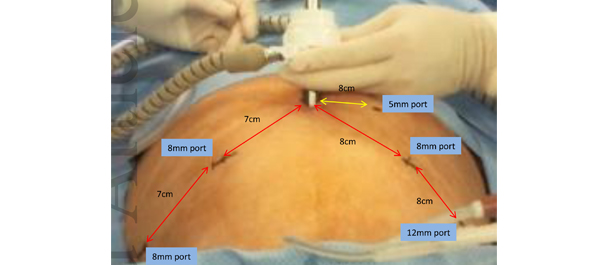
• We retrospectively evaluated data from 202 consecutive patients with non-metastatic upper urinary tract urothelial cell carcinoma (UUT-UCC), who underwent surgery between 1990 and 2012 at a single tertiary academic centre.
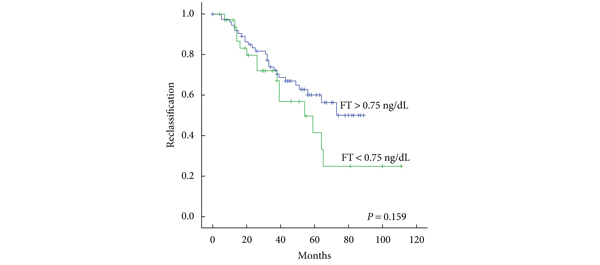
• Patients’ cancer-specific survival (CSS) and overall survival (OS) were assessed using the Kaplan–Meier method.
• To evaluate the independent prognostic significance of the NLR, multivariate proportional Cox regression models were applied for both endpoints.
RESULTS
• A higher NLR was significantly associated with shorter CSS (P = 0.002, log-rank test), as well as with shorter OS (P < 0.001, log-rank test).
• Multivariate analysis identified a high NLR as an independent prognostic factor for patients’ CSS (hazard ratio 2.72, 95% CI 1.25–5.93, P = 0.012), and OS (hazard ratio 2.48, 95% CI 1.31–4.70, P = 0.005).
CONCLUSIONS
• In the present cohort, patients with a high preoperative NLR had higher cancer-specific and overall mortality after radical surgery for UUT-UCC, compared with those with a low preoperative NLR.
• This easily identifiable laboratory measure should be considered as an additional prognostic factor in UUT-UCC in future.