Article of the Month: Progression and treatment of incident lower urinary tract symptoms (LUTS) among men in the California Men’s Health Study
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
This week we feature a video from Dr. Steven Jacobsen discussing his paper.
If you only have time to read one article this week, it should be this one.
Progression and treatment of incident lower urinary tract symptoms (LUTS) among men in the California Men’s Health Study
Lauren P. Wallner, Jeff M. Slezak*, Ronald K. Loo†, Virginia P. Quinn*, Stephen K. Van Den Eeden‡ and Steven J. Jacobsen*
Department of Medicine and Comprehensive Cancer Center, University of Michigan, Ann Arbor, MI, *Department of Research and Evaluation, Kaiser Permanente Southern California, †Department of Urology, Southern California Permanente Medical Group, Pasadena, CA, and ‡Division of Research, Kaiser Permanente Northern California, Oakland, CA, USA
OBJECTIVES
To characterise the progression and treatment of lower urinary tract symptoms (LUTS) among men aged 45–69 years in the California Men’s Health Study.
PATIENTS AND METHODS
A total of 39 222 men, aged 45–69 years, enrolled in the Southern California Kaiser Permanente Health Plan were surveyed in 2002–2003 and again in 2006–2007. Those men who completed both surveys who did not have a diagnosis of benign prostatic hyperplasia (BPH) and were not on medication for LUTS at baseline were included in the study (N = 19 505). Among the men with no or mild symptoms at baseline, the incidence of moderate/severe LUTS (American Urological Association Symptom Index [AUASI] score ≥8) and odds of progression to severe LUTS (AUASI score ≥20) was estimated during 4 years of follow-up.
RESULTS
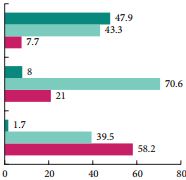
Of the 9640 men who reported no/mild LUTS at baseline, 3993 (41%) reported moderate/severe symptoms at follow-up and experienced a 4-point change in AUASI score on average. Of these men, 351 (8.8%) had received a pharmacological treatment, eight (0.2%) had undergone a minimally invasive or surgical procedure and 3634 (91.0%) had no treatment recorded. Men who progressed to severe symptoms (AUASI score ≥20; n = 165) were more likely to be on medication for BPH (odds ratio [OR] 8.09, 95% confidence interval [CI] 5.77–11.35), have a BPH diagnosis (OR 4.74, 95% CI 3.40–6.61) or have seen a urologist (OR 2.49, 95% CI 1.81–3.43) when compared with men who did not progress to severe symptoms (AUASI score <20).
CONCLUSION
These data show that the majority of men who experienced progression did not have pharmacological or surgical therapy for their symptoms and, therefore, may prove to be good candidates for a self-management plan.