Editorial: Prostate Artery Embolization
Andrea Tubaro, in his editorial for European Association of Urology 2006 [1], discussed the paradigm shift in the surgical management of BPH from open surgery to TURP, and postulated that more refined and less invasive techniques would further dictate the treatment pathway to reduce cost, manage more high-risk surgical cases and reduce blood loss in a population that increasingly is on antithrombotic and anticoagulant medication, to ease the management of large prostates, and to manage BPH as a day case procedure [1].
Interventional radiology has been at the forefront of minimally invasive procedures. In 1953, Seldinger [2] published his ingenious method of introducing a catheter into the vascular system after obtaining needle access and, 10 years later, Dotter recognized the potential of catheters to be used in performing intravascular surgery [3]. Superselective prostate artery embolization (PAE) was first described by DeMeritt et al. [4]. Pisco et al. [5] from Portugal and Carnevale et al. [6] from Brazil have rightly been credited with the development of the clinical service for PAE in BPH. The study by Pisco et al. in 2016, in 630 consecutive patients with moderate to severe LUTS refractory to medical therapy for at least 6 months, showed 81.9% medium-term and 76.3% long-term clinical success rates, with no urinary incontinence or sexual dysfunction reported. Carnevale et al. [6], in 2014, described a modified PAE technique that can lead to greater ischaemia and infarction of the prostate gland with the possibility of better clinical outcomes [6].
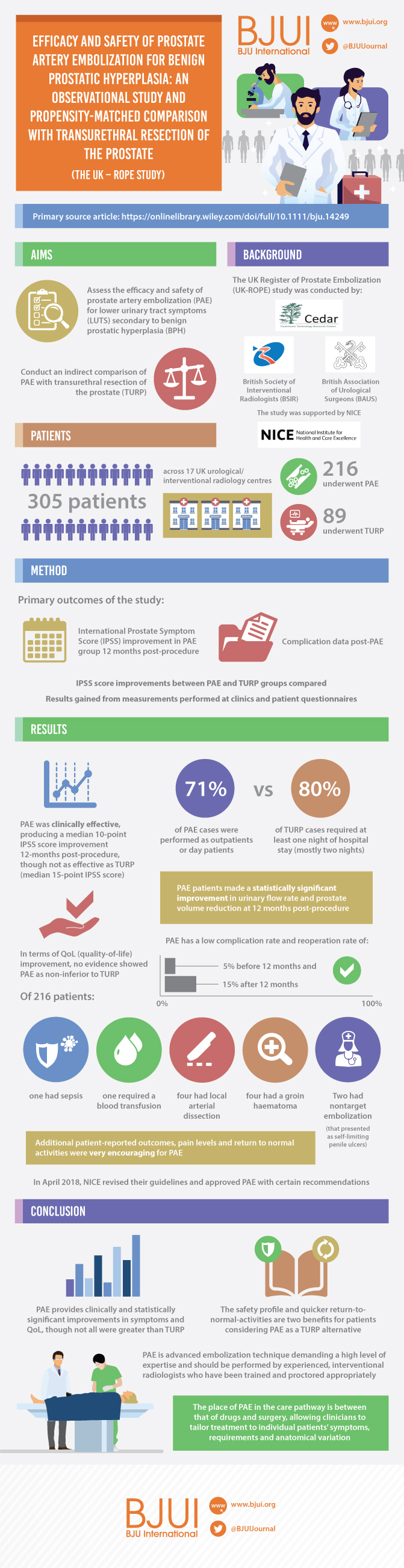
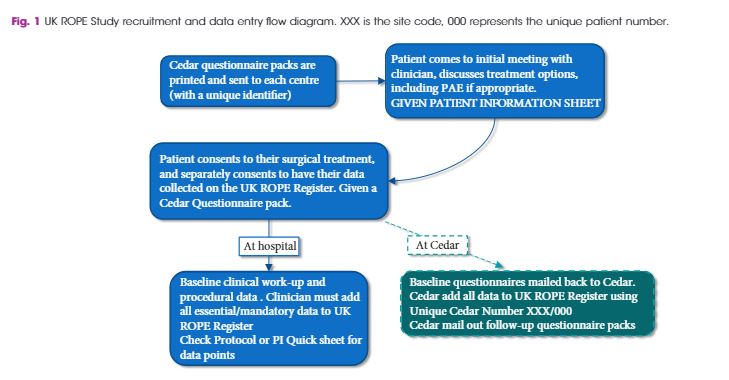
In this edition of BJUI, the UK Register of Prostate Embolization (ROPE) study [7] provides evidence for the efficacy and safety for PAE for LUTS secondary to BPH and makes an indirect comparison with TURP. What is strikingly unique and to be applauded in this registry is the collaboration between the British Society of Interventional Radiology, the BAUS and National Institute of Clinical Excellence (NICE).
A total of 305 patients across 17 UK centres were enrolled, and results were analysed over 12 months. They noted that patients who underwent PAE had a statistically significant improvement in urinary flow rate and reduction in prostate volume after the procedure. In terms of IPSS and quality-of-life improvement, there was no evidence of PAE being non-inferior to TURP. Seventy-one percent of PAE cases were performed as outpatients or day cases. By contrast, 80% of TURPs required at least one night of hospital stay and a majority two nights [7].
In April 2018, NICE revised their guidelines and have now approved PAE with certain recommendations [8].
The key to successful PAE, in our opinion, is careful patient selection. At our centre, we receive tertiary referrals of patients with very large prostates, many of whom are comorbid and elderly. We embraced the option of PAE and were delighted to be able to contribute a number of cases to the ROPE study. Our overall experience is now in excess of 200 cases and we are aware that some patients will do well, others less well. It is becoming clearer who those patients may be; those who do well tend to be those with the larger prostate with large lateral lobes and adenomatous predominant BPH, without a significant middle lobe, with big prostate vessels and with lower risk of significant renal insufficiency. The large middle lobes can ball-valve and still obstruct, and preoperative arterial CT could identify those with heavily calcified, severely diseased internal iliac arteries that may be difficult to embolize. Nonetheless, those patients who are at highest risk from surgery and those who wish to minimize the risks of sexual dysfunction or incontinence may justifiably opt for PAE as a less invasive outpatient procedure. And why should they not? For many, simply the opportunity to avoid long-term medication with a-blockers or 5-a-reductase inhibitors is the real benefit, and undergoing PAE does not exclude one from surgery afterwards.
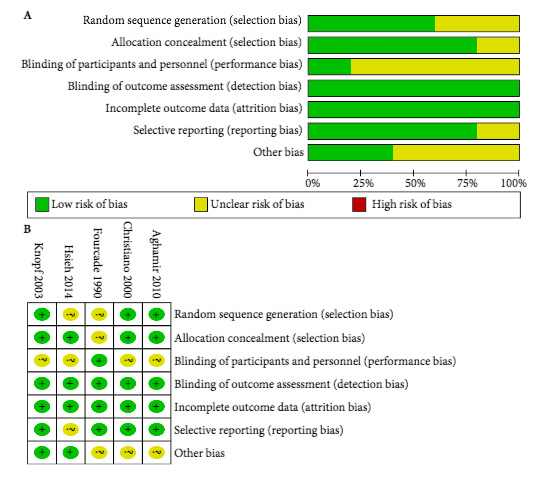
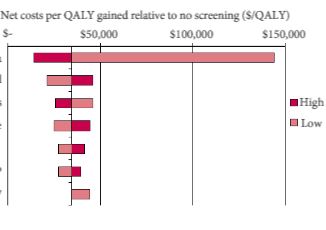
Level 1 evidence is of course a fundamental requirement for a change in definitive practice; the ROPE study is a comparative cohort of two fundamentally different procedures. Our institute is a surgical centre for the management of massive BPH and we are convinced that PAE has a place in the management of some of our patients, but could prevention be better than cure? Ambitious it may be, but who is to say whether early PAE in symptomatic patients might reduce the progression of clinical BPH, avoiding the morbidity and cost of long-term medical treatment culminating in surgery. Perhaps the real challenge highlighted by the ROPE study is that the time has come to consider a randomized controlled trial of prostate embolization vs early non-surgical treatment of BPH (short title ‘PREVENT-BPH’), with randomization to PAE or either a-blockers and/or 5-a-reductase inhibitors or placebo. The ROPE study suggests that PAE at the least deserves a randomized controlled trial including it vs other non-invasive treatments.
Tarun Sabharwal and Rick Popert
Guy’s and St Thomas’ Hospital, London, UK
References
- Tubaro A. BPH treatment: a paradigm shift. Eur Urol 2006; 49: 939–41
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol 1953; 39: 368–76
- Dotter CT, Judkins MP. Transluminal treatment of atherosclerotic obstructions: description of a new technique and preliminary report of its applications. Circulation 1964; 30: 654–70
- DeMeritt JS, Elmasri FF, Esposito MP, Rosenberg GS. Relief of benign prostatic hyperplasia-related bladder outlet obstruction after transarterial polyvinyl alcohol prostate embolization. J Vasc Interv Radiol 2000; 11: 767–70
- Pisco JM, Bilhim T, Pinheiro LC et al. Medium-and long-term outcome of prostate artery embolization for patients with benign prostatic hyperplasia: results in 630 patients. J Vasc Interv Radiol 2016; 27: 1115–22
- Carnevale FC, Moreira AM, Antunes AA. The “PErFecTED Technique”: proximal embolisation first, then embolise distal for benign prostatic hyperplasia. Cardiovasc Intervent Radiol 2014; 37: 1602–5
- Ray AF, Powell J, Speakman MJ et al. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int 2018; 122: 270–82
- NICE Guidance. Prostate artery embolisation for lower urinary tract symptoms caused by benign prostatic hyperplasia. BJU Int 2018;121: 825-34