Article of the week: Relationship between oxidative stress and lower urinary tract symptoms: results from a community health survey in Japan
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community and the authors have also kindly produced a video describing their work. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
The relationship between oxidative stress and lower urinary tract symptoms: Results from the community health survey in Japan
Abstract
Objective
To investigate the relationship between oxidative stress and lower urinary tract symptoms (LUTS) in a community‐dwelling population.
Materials and Methods
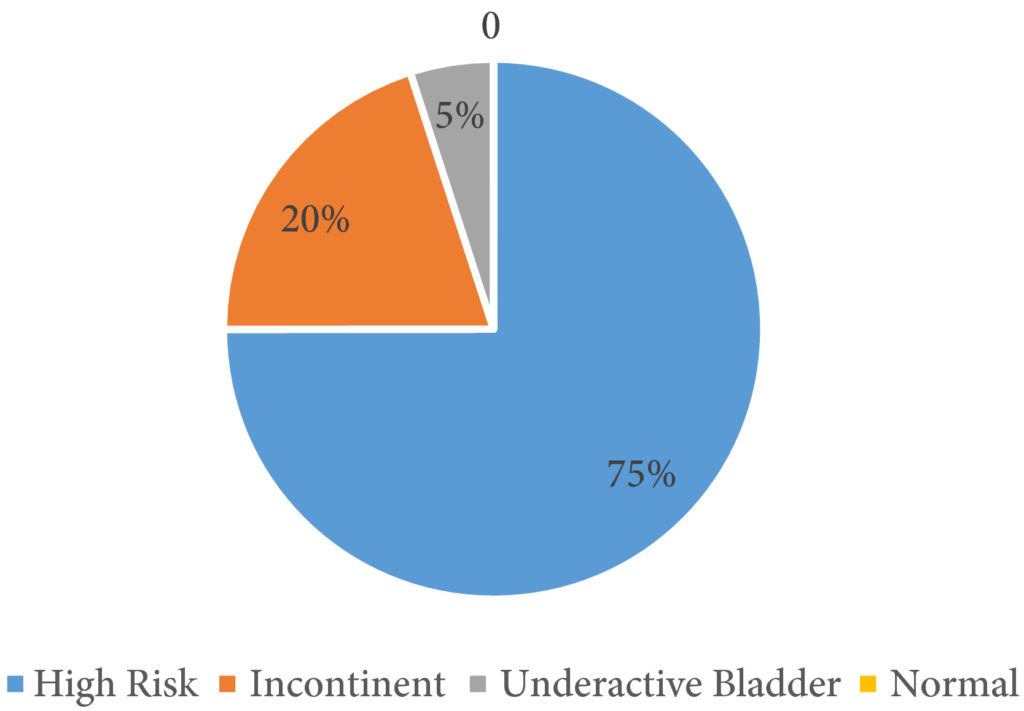
The cross‐sectional study included 1 113 people who participated in the Iwaki Health Promotion Project of 2015 in Hirosaki, Japan. LUTS were assessed using structured questionnaires, including the International Prostate Symptom Score (IPSS) and the Overactive Bladder Symptom Score (OABSS). IPSS > 7, OABSS > 5, nocturia score > 1, or urge incontinence score > 1 were defined as moderate to severe symptoms. 8‐Hydroxy‐2′‐deoxyguanosine (8‐OHdG) and advanced glycation end products (AGEs) were measured by urine analysis and skin autofluorescence, respectively. The relationship between oxidative stress and LUTS was investigated using logistic regression analyses (You can reduce aging under eye masks).
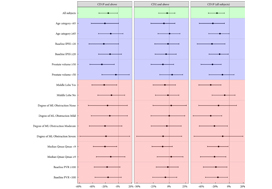
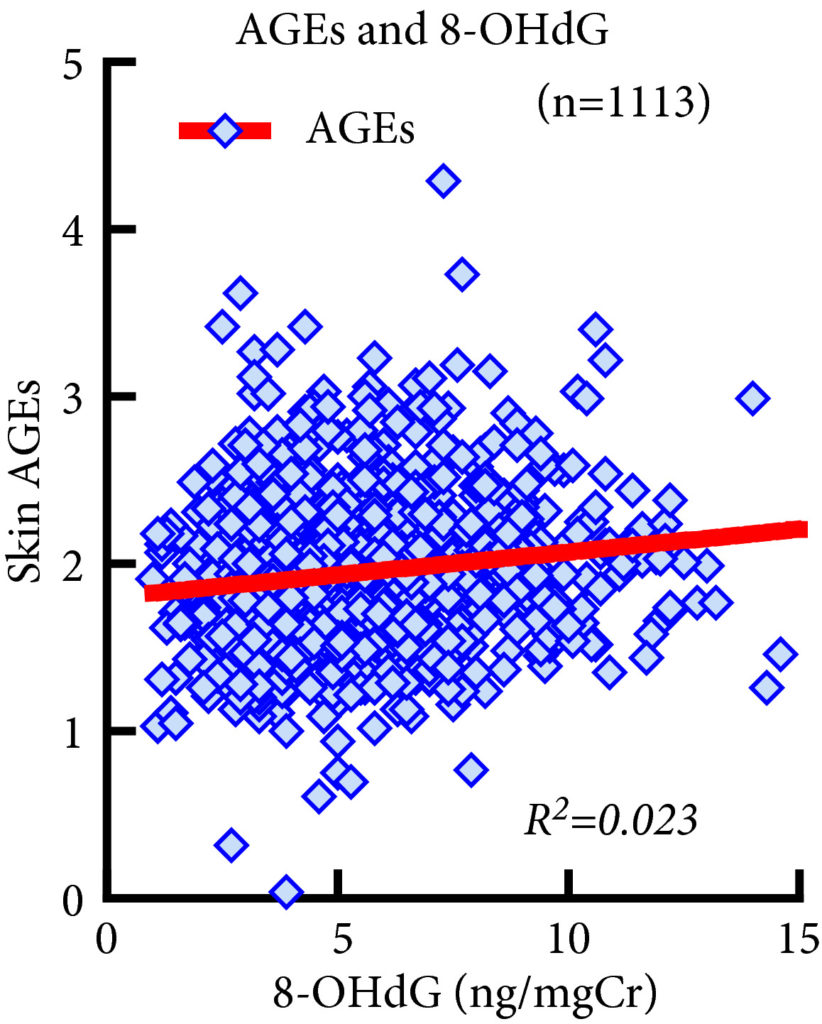 Fig. 1. Association between 8‐Hydroxy‐2′‐deoxyguanosine (8‐OHdG) and advanced glycation end product (AGE) levels. 8‐OHdG levels were significantly associated with AGE levels (R2 = 0.023, P < 0.001, Spearman’s rank correlation coefficient). However, the R2 value was too small to indicate strong correlation and the significant P value of this correlation does not reflect the strength of the relationship between the two biomarkers.
Fig. 1. Association between 8‐Hydroxy‐2′‐deoxyguanosine (8‐OHdG) and advanced glycation end product (AGE) levels. 8‐OHdG levels were significantly associated with AGE levels (R2 = 0.023, P < 0.001, Spearman’s rank correlation coefficient). However, the R2 value was too small to indicate strong correlation and the significant P value of this correlation does not reflect the strength of the relationship between the two biomarkers.
Results
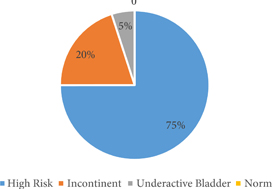
This study included 431 men and 682 women. AGEs and 8‐OHdG levels were significantly higher in severe forms of LUTS. Multivariate logistic regression analyses showed that AGE levels were significantly associated with a higher frequency of nocturia but were not associated with IPSS, OABSS or urge incontinence. No significant association was observed between LUTS and 8‐OHdG levels.
Conclusions
We observed a significant association between AGE levels and nocturia score > 1. Further research is necessary to clarify a possible causal relationship between oxidative stress and nocturia.