The optimal treatment of patients with localized prostate cancer: the debate rages on
The widely anticipated results of the ProtecT study have now been published. Unfortunately, the results do little to advance our understanding as to whether surgery or radiation provides better outcomes.
In summary
The study followed oncologic and functional outcomes of 545 patients randomized to active monitoring (surveillance), 553 to radical prostatectomy, and 545 to radiotherapy. With a median follow-up of 10 years, the authors report no significant differences in prostate cancer specific (p=0.48) or overall survival (p=0.87) among the three treatment groups. They did demonstrate an increase in disease progression and metastasis among men managed with surveillance.
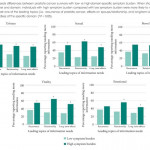
In an accompanying manuscript, the authors examined patient reported outcome measures out to 6 years following treatment. The authors report worse urinary continence and erectile function following surgery and worse voiding symptoms and bowel function following radiotherapy.
What do we take from this?
The investigators and participating patients should be congratulated for successfully completing this study. Numerous authors have documented their failure to adequately accrue to randomized studies of surgery versus radiotherapy in localized prostate cancer (including MRC PR06 and SPIRIT). The failure of these trials, among others, prompted Dr. Wilt to ask “Can randomized treatment trials in early stage prostate cancer be completed?” These authors have unequivocally proven that the answer is “yes”.
However, there are many caveats in applying these results to our patients:
(1) Study power
The study was clearly underpowered to evaluate the primary outcome of prostate-cancer specific mortality. Drs. Roobol and Bokhorst eloquently described important limitations of the ProtecT study. The authors designed the study assuming prostate cancer mortality of 15% at a median follow-up of 10 years. This was later adjusted downwards to 10% based on updated UK data. In the end, rates were closer to 1%. The conclusions of the primary analysis are based on a total of 17 (17!!) deaths.
(2) Study cohort – enriched with low risk disease
Among the randomized patients, the median PSA was 4.6 ng/mL, 76% had clinical stage T1c disease, and 77% had Gleason score 6 disease. These patients would almost certainly be considered most suitable for active surveillance, rather than active therapy, if seen in clinic today. Clinically meaningful decisions between surgery and radiotherapy are in the realm of treatment of intermediate and high-risk localized prostate cancer and these comprise a small group in this study. Based on this baseline distribution, it will be unlikely that any significant differences will be found in future follow-up studies.
(3) Outcomes for active surveillance
Perhaps the most notable findings of this study involve the significantly higher rates of progression, metastasis and prostate cancer specific mortality for patients treated on the surveillance protocol as compared to those treated actively, though statistical significance was not reached for PCSM. The manuscript does not provide further details regarding the pathologic characteristics of these patients. Relevantly, what was the Gleason score for these patients? This is of particularly importance as many surveillance proponents are advocating an expanding role of AS.
(4) Treatments administered
RCTs typically require significant periods of accrual, follow-up and analysis. As a result, they may be out of date prior to completion. This is certainly true of the ProtecT study. This most prominently affects patients allocated to radiotherapy. In the study protocol, patients received 3D conformal radiotherapy at 74 Gy, not the IMRT which has now become widely used. Thus, proponents of radiotherapy will likely to discount any findings which do not favour radiotherapy.
In addition, the current day relevance of the surgical treatment provided is questionable. First, the vast majority of patients in the surgical arm underwent open RP. More concerning is the quality of surgery provided: 93 patients (24%) of the cohort had positive surgical margins. In contemporary series, the average rate is under 15% with centers of excellence approaching 5%. While PSM rates clearly affect oncologic outcomes, they likely are also a surrogate of surgical quality which may affect functional outcomes.
(5) Comparison of active treatments
In the accompanying editorial, Dr. D’Amico comments on a “trend favouring radiation and ADT over surgery” and suggests that “one may consider radiation and ADT as a preferred option”. The basis for this conjecture is 5 deaths in the surgery group and 4 in the radiotherapy group, hardly a convincing sample. In contrast to these data, there was a higher number of patients with metastasis among those treated with radiotherapy (16 vs 13). These discordant results would certainly suggest that any preference for radiotherapy is premature. Indeed, with additional follow-up one would expect the patients with metastasis to die of prostate cancer, thus favouring those treated surgically.
On a methodological note, while the inclusion of active surveillance is a strength of the study, it poses analytic difficulties. The primary analysis assesses a null hypothesis assuming equality across all study interventions. Thus, as this was non-significant, pairwise testing of surgery and radiotherapy, and each with surveillance, is inappropriate and conclusions on these comparisons should not be drawn.
(6) Functional outcomes and treatment-related complications
Most clinicians are well aware that many complications other than erectile function and urinary incontinence may affect that life trajectory of patients following prostate cancer treatments. ProtecT offers the opportunity to examine the risks of secondary malignancy, repeat urologic and gastrointestinal interventions, surgeries and hospitalizations following treatment. However, these are not currently included in the published data.
Further, the PCOS studies have clearly shown that differences in patient reported urinary, sexual and bowel function change over time with convergence after long term follow-up (15 years). With ongoing maturity, it will be interesting to see if a similar pattern emerges in ProtecT.
In conclusion
The ProtecT study may raise more questions than it answers. Among a low risk group of patients, it has shown that active treatment of PSA-detected prostate cancer can reduce the progression to metastatic disease. Assessment of prostate cancer specific and overall mortality, as well as the comparative efficacy of surgery and radiotherapy, is not possible due to power limitations.
Will you be changing you patient counselling based on these results?
| Christopher Wallis, MD Resident, Division of Urology, Department of Surgery, University of Toronto Doctoral Student in Clinical Epidemiology and Health Care Research, Institute of Health Policy, Management & Evaluation University of Toronto |
|



Great blog Chris and Rob, and congratulations to all the ProtecT team for designing and recruiting this landmark study.
This and the recent Brisbane RCT of open vs robotic RP (https://www.bjuinternational.com/bjui-blog/its-not-about-the-machine-stupid/) are stark reminders of how difficult it is to run RCTs of surgical practice. ProtecT is a particularly impressive study, but as it was designed 20 years ago, it therefore asks a question that has less relevance in clinical practice. If the authors were asking a similar question today, they surely would not have allowed 77% of patients to have Gleason 3+3=6 cancer. The study therefore is not powered to to answer the question of most relevance to localised prostate cancer today – that is, what is the value of intervention in a screen-detected population of clinically significant prostate cancer.
Nonetheless, a wonderful study, which will be interpreted in many different ways depending on perspective. Congratulations to all investigators.
Great blog–congrats. For you last question–I will only modify my counseling for active surveillance to reinforce that a single biopsy and PSA trending will not be adequate enough to select and monitor with success. But we mostly believe this to be true and would offer/recommend scheduled repeat biopsies, MRI staging, targeted biopsies when appropriate, and possibly genomic testing. Given the high enrollment of low grade biopsies and follow up at 10 years, I will not modify any messaging related to surgery vs radiation questions–the trial is inadequate to answer any of these questions and frankly surprised with D’Amico’s “reach” at using a high profile editorial to argue results with minuscule number of events and not statistically significant.
An excellent summary of a complex and challenging study. Because active surveillance is so widespread these are the group of patients we are most interested in treating. We hope further data can tease out those at risk of progression. The more aggressive we become with active surveillance the more wary we must be of incorrectly assigning risk. Notably MRI is now a strong discriminator and was not part of the trial.
Further as was pointed out in a multidisciplinary meeting just this week by both a radiation oncologist and endocrinologist if considering active treatment we must consider surgical monotherapy versus radiation plus neoadjuvant hormonal therapy (ADT). This was the treatment offered in the ProtecT trial. We should no longer be stating “radiotherapy” implying monotherapy without mentioning hormonal therapy because this carries with it more significant side effects. If ever the hormonal component is dropped from treatment we may go back to stating “radiation alone” or “radiotherapy”. The men’s health clinic have noted prolonged effect of even 6 months of ADT meaning testosterone recovery is not guaranteed now posing problems of replacement or not in the setting of active cancer.
These are good points we should all consider.
Great blog and many congratulations to the ProtecT team for this work – successful completion of an RCT in localised prostate cancer study is a huge achievement.
We have known for some time that PSA monitoring alone on active surveillance is not enough. Some address this with regular biopsies schedules with others adding in MRI imaging to identify those with more significant disease at outset, and to identify change in disease as it occurs. Each of these will have a significant impact on outcomes, although more work is needed to look at how repeat MRI in men on active surveillance should be used, and how cost effective this will be.
For counselling men in clinic – the extremely low mortality overall despite selection using PSA and standard biopsy, the similarity of oncological outcomes for active treatment and the difference in the type of side effects between radiotherapy (with short term ADT) and surgery will all need to be discussed.
Great blog Chris and Rob and extremely pertinent points. It is become clear that the demographics of men undergoing prostate cancer treatment has shifted in the last 10 years to a far higher proportion of intermediate and high risk disease – as it should, in response to the evidence supporting a conservative approach in low risk disease. Unfortunately ProtecT adds to the evidence supporting conservative management of low risk prostate cancer but gives no useful information regarding treatment efficacy in the very patients that require the best treatment. If PIVOT has confirmed no advantage to surgery over surveillance in men with largely low risk disease, why would ProtecT be expected to show any benefit of either surgery or radiation therapy in a group of men that had a 1% cancer-specific mortality rate at 10 years??
It will be dangerous to erroneously extrapolate ProtecT results in order to counsel young men with high grade disease that there is no survival benefit from surgery over radiation when in fact all available evidence up until now has shown otherwise, as Wallis and Nam et al have recently demonstrated through their meta-analysis. Unfortunately the lay media are misrepresenting these results already which simply adds more confusion to the debate – the conclusion that should be clearly emphasised is that ProtecT is a well designed RCT of patients with largely low risk disease confirming that active surveillance is the most appropriate option for most of these men.
How can you compare a retrospective “meta-analysis” with its selection bias to the randomized level I ProtecT data? You simply cannot. The ProtecT data trumps retrospective series, including the Wallis paper, and it isn’t a close call by any means.
Chris and Rob — very nice dissection of the manuscript.
Huge kudos to the authors and participants for doing what many stated would never be possible.
To me the, the difference between the “No treatment” (not truly AS) and the Treatment groups actually is a bit of a relief that speaks to the fact that our current treatments are actually moving the needle for those that need to be treated.
What’s not clear to me from the manuscript is what were the clinicopatholigic characteristics of the patients who progressed? Was higher risk of progression in the “No treatment” arm due to the 23% of patients who had >Gleason 6 disease. To this end, a Table similar to the existing Table 2
(https://www.nejm.org/na101/home/literatum/publisher/mms/journals/content/nejm/0/nejm.ahead-of-print/nejmoa1606220/20160914/images/large/nejmoa1606220_t2.jpeg) , which outlines progression (not death) according to subgroup would have been helpful.
I hope that subanalysis is in the near future.
Regardless, glad to see us starting to emerge from the Dark Ages with these Level 1 data.
Great blog. Yes, it’s a RCT, but what to do with the conclusions of this study in the clinic? Personally I think that we nowadays have better staging modalities and do a better selection of patients who can safely start with an active surveillance program. And yes, surgical approach and radiation protocols also changed in the last 10 years. Keep that in mind when discussing these study results with your patients
Seems unfair to misrepresent Dr. D’Amico like that. That statement was entirely contingent on further results. He does recommend men choose a treatment based on their expectations of the effect on qol. Iow, which would you prefer, pads and ed, or the occasional bloody bm?
Speaking as a patient diagnosed yesterday (3+4, pondering), that is nicely impartial!
I always appreciate randomised controlled trials of prostate cancer related treatments. Even when the results are of limited direct significance the detailed data can provide a relatively unbiased way of looking at the frequency of various outcomes (e.g. in patient discussion groups I often refer to the erectile dysfunction results from a randomised trial of prostatectomy techniques), and non-inferiority results are really helpful for the patient because they give freedom to chose.
As a prostate cancer patient deciding on treatments I want to know the outcomes for patients in my situation. That makes me very much want at least an analysis of the progression results for each intervention by Gleason score, including division into Gleason 3+4 and 4+3. The Gleason 7+ patients are swamped by the Gleason 6 ones. There were more non-compliant patients than there were Gleason 7+.
Given the levels of non-compliance with the protocol I’d also like to see an analysis by actual treatment, as well as the more formally valid intention to treat already published.
Overall I felt this study recruited a lot of low-risk patients many of whom were over treated by current standards. I pity them. I’m very glad we now have active surveillance protocols for them.
Sadly I’m already seeing media articles saying this study shows treatment makes no difference.
https://www.theage.com.au/national/survival-rate-for-early-prostate-cancer-just-as-high-if-men-skip-treatment-20160915-grgr91.htmlhttps://www.bbc.com/news/health-37362572
Since 40% of the Active Monitoring group had treatment within 5 years and 56% within 10, this is more of a early versus delayed treatment result. Since the group was dominated by low risk patients it is not an accurate reflection of the risk from undiagnosed prostate cancer. I fear more men will forgo PSA testing, as I did, because of this sort of media report. My testing omission, despite a PSA of 3.3 at age 47, gave me a 20cc T3a tumor when detected at 52 more or less unintentionally.
Well done ProtecT team clearly a massive undertaking and great to see it published. The UK newspapers and media have grasped a single message from the trial unfortunately and to quote the BBC ‘Prostate Cancer Treatments Overused’ will misinform the general public. Clearly significant cancer does need treatment and patients should not assume all prostate cancer is suitable for surveillance.
The trial really supports current up to date practice in as much as we don’t treat low risk disease and active surveillance protocols are robust in ensuring progression is not missed and treatment can be given in a timely way.
Congratulations to the ProtecT authors on their tremendous effort completing a randomized trial comparing treatment strategies and collecting long-term patient-reported outcomes- an extremely important contribution!
With respect specifically to the conservative arm of the study, the take-home message might be interpreted by different readers in divergent ways – “active monitoring is safe” because there were few deaths overall and no statistically significant difference, versus “active monitoring is not safe” because there were more metastasis in that group. I agree with Caroline Moore’s comment regarding the “active monitoring” in this study, which is very different from the way that “active surveillance” is currently performed. Contemporary prospective AS cohorts use more strict eligibility criteria and monitoring protocols, including not only PSA changes but also regularly scheduled DRE, biopsies, and increasingly other new tests like MRI. I agree that more data are needed on MRI use during AS, but there is no question that it helps to identify cases with occult higher grade disease. Our group has previously shown that PSA kinetics are not a reliable predictor of underlying disease reclassification (https://jco.ascopubs.org/content/early/2010/05/03/JCO.2009.25.7311.abstract), so follow-up biopsies (unfortunately) remain an important component of an active surveillance protocol. Although it is not possible to prove the counterfactual, I do suspect that the rate of metastasis would have been lower in the “active monitoring” group if they were selected and monitored in line with contemporary protocols.
The most important take-home message from this study is that every decision has important trade-offs. Each option for prostate cancer treatment has clear pluses and minuses, so individual patient characteristics and preferences should be assessed in an effort to help them choose the best option.
Thanks.
The debate certainly should not be raging on.
We now have level 1 evidence to change our practices, which combined with PIVOT and SPCG-4, point to very straightforward practice changes that should occur immediately everywhere, if they haven’t already:
1. Men diagnosed with low risk prostate cancer can be safely managed with active surveillance.
2. It is even more safe to manage low risk men on active surveillance in a modern diagnostic and surveillance pathway incorporating mpMRI and biopsies. I would go as far as to argue that it is a medical error to radically treat such men and we should all stop trying to justify this on the basis of patient choice. All the harms and no survival benefit – I think our counselling is at fault if a patient still chooses radical therapy.
3. Surgery is no better than radiotherapy and vice versa. Selective use of positive margin data from case series to dismiss countless experienced open surgeons’ data in PROTECT is wrong. Arguing that radiotherapy is nowadays better is equally wrong.
4. If you’re going to treat intermediate risk men with radical approaches, they had better fully appreciate that the therapeutic ratio is tight (significant harms, a small benefit), even in the best of hands.
…and the accompanying NEJM editorial … truly disappointing.
A truly impressive study. Chris and Rob – great blog post. I would echo the sentiments of those above – I am most interested in those men in the active monitoring group who developed metastatic disease. What where their disease characteristics? Would those men have been candidates for AS in the present time?
Despite the limitations, the study clearly lends credence for AS in appropriate men with low risk prostate cancer. Despite what Dr. D’Amico stated in his editorial, the study clearly does not support that radiation is preferred over surgery (or vice versa).
Well done to the authors of both the paper and the blog. Maybe the take home message is that with the pace of investigational technology, let alone treatment, RCTs for treatment of prostate cancer are redundant in the 21st Century. By the time we have robust survival data (10 years plus), the diagnostics, treatment group, and treatments are no longer relevant to contemporary practice. Does anybody have an idea for an effective alternative?
Impressive era where RCTs in prostate cancer apparently become standard practice! Sincere respect for the authors. Nevertheless striking that such level 1 evidence isn’t the highly anticipated light at the end of the tunnel.
We will probably continue to operate the young guys and irradiate the old guys.
As for active surveillance … a urologist told me his New Years’ resolutions were giving up coffee, unhealthy food and active surveillance. Well, the increased rates of metastasis and disease progression in a mainly low risk population where 55% of AS patients received active treatment … even knowing that today is different … that’s still pretty scary. So eagerly awaiting subgroup analysis, meanwhile having another coffee.
Well – this was the study we all said couldn’t be done. ProtecT really challenges us all to be ambitious in trying to answer thorny questions in Uro-oncology through properly constructed clinical trials rather than relying on lower level evidence. Just because these trials are hard, doesn’t mean they shouldn’t be done, and certainly once appropriate randomized trials become available for our patients, we should all try to support their accrual.
A key criticism is that only ~25% of men in ProtecT were intermediate risk, and that the majority of patients accrued would currently be offered Active Surveillance. Important lessons can still be learnt. Most importantly is that the hazard ratio for all relevant disease control outcomes between radiotherapy and surgery was unity. This is certainly true for low risk disease, and possibly also for intermediate risk. Note that this is in complete contradistinction to the plethora of registry level publications, including from the authors of this blog, suggesting a major advantage for surgery, even for low risk disease (see https://www.europeanurology.com/article/S0302-2838(15)01160-4/abstract/surgery-versus-radiotherapy-for-clinically-localized-prostate-cancer-a-systematic-review-and-meta-analysis). Given level one evidence against this, we must therefore conclude that the uncontrollable selection biases inherent in such analyses are what leads to the results, rather than any treatment effect.
Hopefully this data will be communicated with our patients, and they will be allowed the opportunity to explore proven alternative treatments prior to making a final treatment decision.
Congratulations to Professors Hamdy, Donovan and Neal and the whole of the ProtecT team for delivering this fantastic study. I have heard Professor Hamdy speak with eloquence of the journey taken with ProtecT, particularly the early challenges to randomise (Donovan et al, 2003 – https://www.journalslibrary.nihr.ac.uk/__data/assets/pdf_file/0011/64928/FullReport-hta7140.pdf), and it is impressive that equipoise was achieved to such an extent that the greatest proportion of men who accepted their assigned arm in the intention to treat analysis were those assigned to active monitoring (by some margin at 88% compared to 70% and 74%).
This is in the context of 22% of these men having intermediate risk (or a small number even high risk) disease. The limitations of the study have been expertly outlined by Drs Wallis and Nam above, including the preponderance for low risk disease in the study cohort. But it is impressive that even this number of men with non-low risk disease were able to be randomised to monitoring given what we now know about preferred treatment options for this type of disease (SPCG-4, PIVOT etc).
Although some have commented that the AM here is not true AS the authors nonetheless point out that this was very different to the watchful waiting arms of the above trials which had no planned radical intervention for progression. And, as has also been mentioned, it would be interesting to reassess the ProtecT biopsies to see how many of the Gleason 6 tumours are actually Grade Group 2 or 3 on current assessment – this study may be less low risk than we think…and the case for surveillance made stronger in appropriately selected men by subsequent sub-set analyses. As Dr Kutikov states above, it would be interesting to see the Gleason/PSA/T stage breakdown for the progression and metastases outcomes where evidence of a difference was seen. Further subset analyses and longer term survival outcomes (where these secondary endpoints convert to the primary endpoint) will be eagerly anticipated and may provide greater distinction between treatment arms, accepting the historical nature of radiotherapy and prostatectomy in the study (perhaps more relevant for the PROMS paper).
There has also been some discussion of the presence of Gleason 8-10 men in the randomised cohort. As stated in previous ProtecT publications (Lane et al, 2004 – https://www.thelancet.com/pdfs/journals/lanonc/PIIS1470-2045(14)70361-4.pdf) but not repeated here, men with locally advanced disease (cT3-4) or PSA >20ng/ml were excluded from randomisation. As stated in the trial protocol, these men were studied separately providing a unique opportunity to assess the outcomes of treatment (non-randomised) in this cohort of men selected by PSA testing from a background population with very low opportunistic PSA screening (~10%). As can be anticipated, the rate of prostate-cancer-specific deaths is likely to be much higher in this group and should provide some insight into management of this cohort when published.
Congratulations to getting to this point – but the study must continue for another 10 years to be able to provide more meaningful results: Both statistically (larger numbers, will metastasis turn to deaths, will differences between treatments increase or evolve …) and due to the different long-term effects of treatments (radiation may be effective in the short term, but lead to larger long-term adverse effects).
1. Even if not statistically significant, and some “probably” prostate cancer related deaths leave questions, the study results overall suggests better cancer control for “treated” persons.
Many questions were left:
2. The study informs about larger age at entry for persons with death due to prostate cancer (Table 2: only 5/17 = 29% were below 65 years at randomization). With a mean age of 62 in the overall randomized group, prostate-specific death appears to have occurred to the older men more frequently. Can this be explained?
Probably a selection bias occurred as younger men with intermediate risk cancer were reluctant to enroll in a study with the “risk of no treatment” (and/or their physicians supported that), while older men were more willing to participate. The younger participant will also have more time alive to be affected by long-term effects of radiation, another possible reason for them to avoid a randomized study with three possible arms.
3. Active monitoring fares worse for the older persons (7 deaths of 12 from the 65+ year group) than for younger (1 death of 5), even if both results may not be statistically significant.
However, that might similarly be explained by either
(i) younger patients from the active monitoring arm changing to radical treatment more frequently, and even without motivation by progression of PSA or other markers, (i.e., the good results for men “active monitoring 100 ng/ml cases?
7. The percentage of “positive” results in needle biopsies (prior to randomization) – both in respect of percentage of positive needles and the percentage of cancer material in each needle – is another indicator that was not identified in the report. It could, however, also become part of a meaningful division for future allocation to treatment.
8. It should be tried to split “other” deaths and deseases to some extent – some long-term consequences of (e.g.) radiation may be hidden under the “probably not treatment-related” deaths and only be conceivable with statistical analysis.
Conclusion:
I would suggest to perform a separate statistical analysis, distinguishing between
(a) the probably “safest” cases (Gleason 6, T1c AND PSA below 6) [or PSA below 10], or, alternatively, for at least 2 or the 3 criteria, for 62+ years at entry,
(b) the same Gleason 6, T1c and low PSA for below 62 years [or applying another age demarcation that splits group (a) and (b) in similarly large groups], and
(c) the remaining group with higher risk scores.
9. Apart from questions about penetration strength, men should also be asked about the continuation of their marriage or partnership, about divorce and finding of new partners. Different general-health related information (e.g. smoking or obesity) could also be monitored. If wifes quit their husbands due to impotence or incontinence, and that in turn leads to otherwise unhealthy way of life, that also must be counted as treatment-related consequence.
10. Continuation of the study follow-up will be very important. Time will lead to more statistically reliable result also for such smaller groups, due to increased cancer-related death and progression rates.
It was also perceicvable that for the low-risk grades, an advantage of radical treatment in progression will once be statistically visible, while the absolute difference in survival (etc.) was still rather low and still would not merit intervention.
I would like to take this opportunity to congratulate the authors on this interesting trial. Alas, the long awaited results are as we all expected. The majority of these men had low risk disease, and I don’t think any of us expected there to be much of a difference between the groups at 10 years.
Out of 391 men that had surgery; 9 patients had a thromboembolic or cardiac event, 14 were transfused, 1 had a rectal injury and 9 required intervention for anastamotic issues. These are impressive complication rates, however, given that 77% had Gleason 3+3 disease and 76% were clinically T1c, a positive surgical margin rate of 24% seems rather high, although there was no breakdown in the PSM rates for T2/T3 disease.
Regarding any individual interpreting this data; office urologists can say they now have multi-parametric MRIs and strict active surveillance protocols, surgeons can say that they now have potentially better tools (such as a robot), oncologists can now say they have superior technology to administer IMRT.
However, I read this paper early this morning and on my commute to work I had already heard the results being misrepresented on a national radio station.
Congratulation to the authors on a great trial. We seem to agree that RT and surgery are about equally efficacious in this population but not much has been said about the toxicity yet. Is it fair to say that RT was much less toxic, at least where the important toxicities are concerned ?
ProtecT is an amazing research effort, for which the authors should be congratulated. In a fast evolving landscape of prostate cancer, it is inevitable that clinical practice has already evolved at the moment a study is actually completed. The ‘active monitoring ‘ arm (mainly PSA monitoring, re-evaluation only when short PSA-doubling time 20) definitely seems to be more active than ‘watchful waiting’ (and also has a curative intent), but is much less strict than the modern ‘active surveillance’ protocols (and in ProtecT also included 22% Gleason >6 cancers). Especially the standard repeat biopsy (and more recently: new imaging) is considered important in active surveillance, but was not (yet) included in the active monitoring arm of ProtecT. Focus on PSA kinetics only may miss tumor misclassification / true biological progression in an expectant management situation. The outcomes of current active surveillance protocols may therefore be more favorable than suggested by the outcomes of the ProtecT active monitoring arm. At the same time, the beneficial effect of active treatment (either surgery or radiation) over expectant management may be less obvious when compared to active surveillance instead of active monitoring.