sLND for Prostate Cancer Nodal Recurrence: #urojc September 2014 summary
The September 2014 edition of the International Urology Journal Club (#urojc) returned to familiar territory – prostate cancer. In particular, the discussion focused on salvage lymph node dissection following radical prostatectomy. For the second time (first in July 2014), two journal articles were selected. Both were kindly made available to open access by The Journal of Urology (@JUrology).
The first paper from the Mayo Clinic by Karnes et al., titled ‘Salvage Lymph Node Dissection (sLND) for Prostate Cancer Nodal Recurrence Detected by 11C-Choline Positron Emission Tomography/Computed Tomography (PET/CT)’, reported on a retrospective single-surgeon series of 52 men who underwent salvage lymph node dissection for nodal recurrence post radical prostatectomy. Median follow-up was 20 months. Three-year Biochemical recurrence (BCR)-free survival rate was 45.5% (PSA <0.2). Metastatic/systemic progression-free and cancer-specific survival rates were 46.9% and 92.5% respectively. They concluded that sLND may delay further progression of disease but highlighted the need for randomised controlled trials.
The second paper from German group Tilki et al., titled ‘Salvage Lymph Node Dissection for nodal recurrence of prostate cancer after Radical Prostatectomy’, also reported on a retrospective series of 58 patients who underwent sLND for nodal recurrence on PET/CT post radical prostatectomy. Median follow-up was 39 months. All but 1 patient had BCR. Five-year clinical recurrence-free and cancer-specific survival rates were 35.9% and 71% respectively. Tilki et al. concluded that while most patients had BCR, sLND may delay ADT and clinical recurrence in selected cases.
A common sentiment shared during the discussion related to the lack of randomised evidence for sLND:
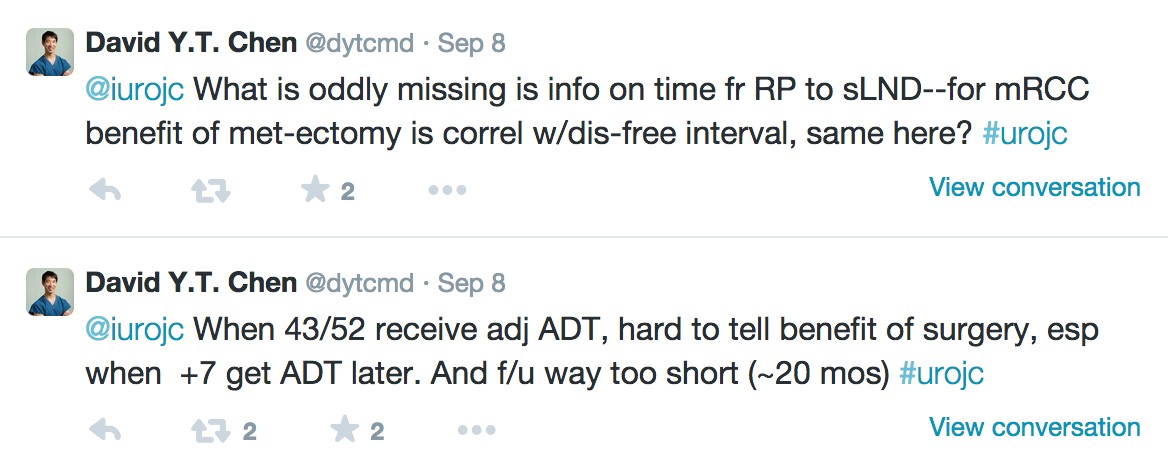
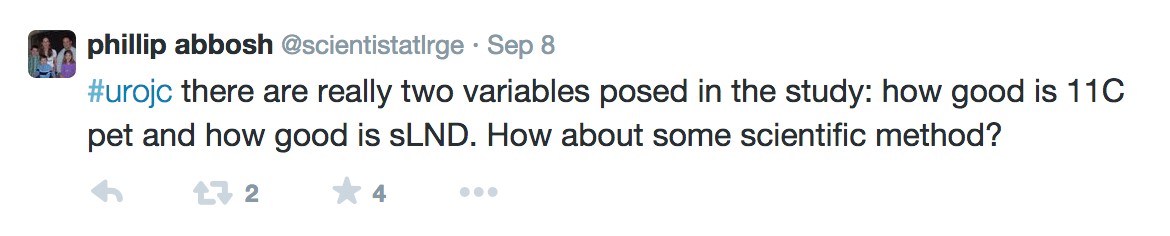
There were some serious concerns about the methodology and results from the two articles:
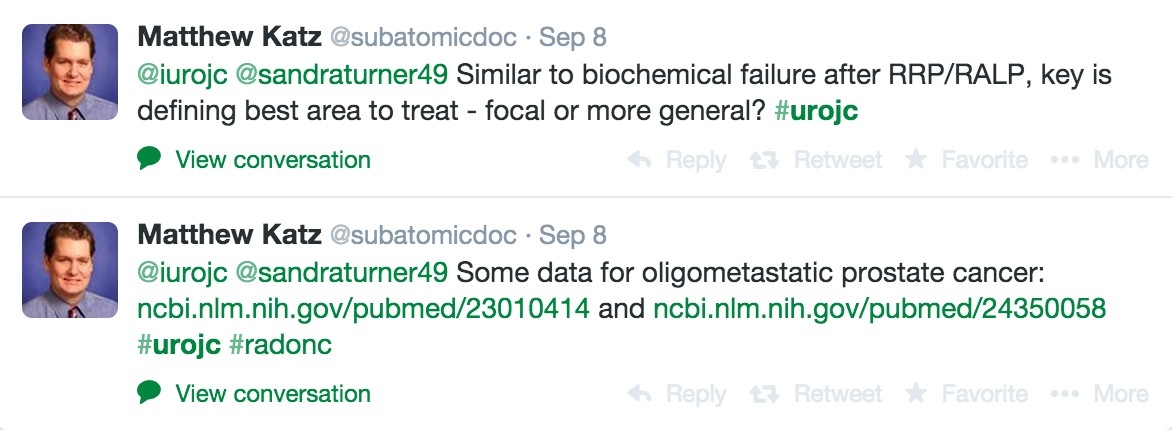
Discussions quickly shifted away from the two articles to the actual clinical question of sLND in oligometastatic disease and delay to ADT. Matthew Katz provided useful links to the use of stereotactic radiation therapy.
Issues surrounding sLND training and the paradigm shift in recent years were also highlighted:
Opinions were divided on the question of surgical morbidity versus the potential increase in time to ADT:
Pop culture references were in vogue this month. An article by the Mayo Clinic on the 11C-Choline PET scan sparked the linked exchange:
Some take home messages pertained to the uncertainty regarding patient selection and the role of sLND in the broader multidisciplinary arena of prostate cancer treatment:
The winner of the Best Tweet Prize is Brian Chapin (@ChapinMD) for his tweet above. We thank the Journal of Clinical Urology for supporting this month’s prize by way of a one year electronic subscription to their journal. We also thank the Journal of Urology for supporting this month’s discussion by way of allowing time limited open access of both articles.
Staying true to form, this month’s edition of #urojc provided a forum for lively international discussion. We look forward to next month’s installment and especially encourage trainees to make use of this excellent educational opportunity.
Isaac Thangasamy is a second year Urology Trainee currently working at the Royal Brisbane and Women’s Hospital, Brisbane, Australia. He is passionate about education and social media. Follow him on Twitter @iThangasamy