Prostate Cancer Outcomes Study Meets Twitter Face to Face
The International Urology Journal Club on Twitter discussion for February 2103 was based upon the recently published Prostate Cancer Outcomes Study in the New England Journal of Medicine on 31 January 2013.
The originally planned discussion paper that was only hours away from being announced when it became apparent through Twitter notification by @NEJM that the PCOS paper was going to be published that day. With this news, ‘urology twitter’ spoke loud and clearly (well, tweeted to be technically correct), and it was clear that this paper required our urgent attention.
The primary and senior authors of the PCOS manuscript in Matthew Resnick and David Penson, respectively, were kind enough to commit to making themselves available for the twitter discussion and proved to be valuable contributors.
In short, PCOS examined 1655 men who had been diagnosed with prostate cancer in 1994 or 1995, between the ages of 55 and 74 years, and who had either undergone radical prostatectomy (1164 men) or radiotherapy (491 men). Functional status was assessed at ‘baseline’ and at 2, 5 and 15 years after diagnosis. The study found patients undergoing surgery were more likely to have urinary incontinence and erectile dysfunction at 2 and 5 years, but there was no significant difference at 15 years. Patients undergoing surgery were less likely to have bowel urgency at 2 and 5 years, but again, there was no discernible distinction between the two groups at 15 years.
The functional results as stated in the manuscript are poor and this generated discussion that attempted to place these results into context. It was pointed out by Stacey Loeb that with the Massachusetts Male Aging Study (MMAS), 79% of men had ED as defined by IIEF and that there was a concern that, with the present data, the media could interpret it as that all prostate cancer treatments universally cause ED. A later constructive comment was made that if the study had followed matched controls to 15 years, it would allow for meaningful estimation of risk with treatment superimposed on aging.
Discussion shifted to the changes that have occurred over time since men entered the study. A number contributors, including Matt Coward, Rajiv Singal, Quoc Trinh and others commented to the effect that many of the men treated in that era would probably no longer be treated radically and would be managed conservatively. Ben Davies in agreement declared that he would promise never to operate on a man with a Gleason score 2–4 prostate cancer. However, Sean Williamson, Alanna Jacobs and others pointed out that this was not really relevant to the study, which was an examination of functional outcomes.
Is the data applicable to today? In response to Tony Finelli’s tweet of “Why is it that the urologic community always criticizes longterm well designed studies with ’The data are no longer applicable today?’“, Rajiv Singal made a very sobering comment that “Data is very applicable. Study well designed. It’s just that over Tx in many in this group makes side effects more appalling”
Prokar Dasgupta provided some British input with “are patients happier if they are clear of cancer @15 years or would they rather be potent?” Michael Leveridge from Canada provided constructive input with “As rational CaPr treatment shifts toward higher risk (wide fields, less nerve sparing), functional outcomes may actually get worse”
Criticism made that there were many men who missed out on completing their 2 and 5 year questionnaires was responded to by Dave Penson who explained that they were included in the study by using imputed data with a hot deck technique – whilst imperfect, it was the best that they could do to overcome this issue.
Stacey Loeb pointed out that a key strength of the study was that it showed that many short-term differences functional outcomes between RP & RT dissipate over time. From a functional perspective, Tim Averch may have a point when he commented that at 15 years that it may not make any difference as to whether we had performed surgery or radiotherapy.
The question was raised about correlating nerve-sparing surgery and subsequent results. Author Matt Resnick indicated that this was something that was being analysed right now with results forthcoming. On the general issue of improvements in surgery and radiotherapy leading to improved functional outcomes, Matt Resnick indicated that “While tech. improvements in RP and EBRT may incrementally improve outcomes, likely non-differential.” Towards the end of the discussion, it was generally agreed that robotic surgery was the primary manner by which surgery was being performed (at least in the US) and that it was an ‘operative leveler’ in terms of how well surgeons performed a radical prostatectomy.
Helen Nicholson from Australia asked if the late serious effects of radiotherapy were considered and on a similar theme, Matt Cooperberg raised the issue of where only incontinence was reported with regard to urinary function but irritative urinary symptoms were often of greater bother and worse with radiotherapy. Dave Penson responded in that they had data on bother from urinary symptoms and that it was worse at 2 and 5 years for surgery but the same for both radiotherapy and surgery at 15 years.
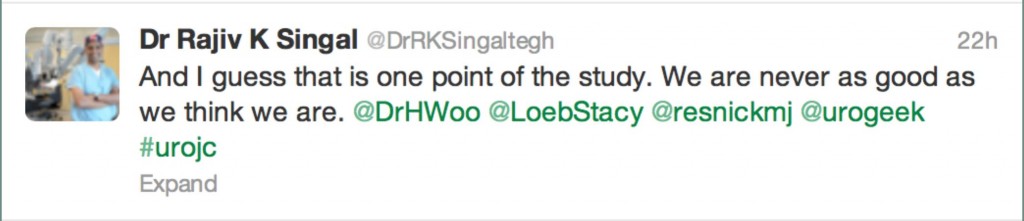
To complete the round up of the discussion content, the Best Tweet Prize was awarded to Dr Rajiv Singal for the following tweet:-
The Best Tweet Prize was kindly donated by Urology Match.
The above summary only touches upon the discussion, which had 32 participants who made a total of 171 recorded tweets to the hashtag #urojc. This does not include participants and their tweets where the #urojc had been omitted. We had quite a number of new participants this month who were still learning the necessity to include #urojc in all tweets in order for them to be visible to the discussion.
It is also interesting to look at the impact of the Superbowl. The first dip is related to our North American friends signing off to concentrate on the Superbowl and the last dip correlates when the majority of participants are with their heads buried in a robot console/wound or asleep on the other side of the world.
We look forward to seeing your participation in the March #urojc. For further information about what #urojc is all about, see my earlier blog entry on the subject.
Henry Woo is an Associate Professor of Surgery at the Sydney Adventist Hospital Clinical School of the University of Sydney in Australia. He has been appointed as the inaugural BJUI CME Editor. He is currently the coordinator of the International Urology Journal Club on Twitter. Follow him on Twitter @DrHWoo
Comments on this blog are now closed.



Great summary Henry. It is great to see social media being used so productively to discuss hot topics like this. There is no other forum which allows this type of discussion and reaction so soon after publication of a major paper. And to have the senior authors engage on Twitter also is terrific. The volume of traffic speaks for itself and I think we will see future #urojc forums growing the engagement even more. We at BJUI are very supportive of this
Declan
Congratulations Henry on this very novel concept! Journal club has always been my favorite conference at our institution, as a great way to stay up-to-date on the latest findings and get different perspectives on the data from colleagues. The new twitter #urojc expands on this concept by allowing a discussion with esteemed colleagues from around the world! Great job in starting this initiative and hopefully it will continue to grow in the future.
Henry, I echo Declan’s comments. I missed most of the Twitter chat this time. One of the problems I find with Twitter is that it is very hard to catch up on if you miss a few days because you are away. I really enjoyed reading this article and which does appear to summarise the discussion very well. I would be in favour of this being a regular blog of the #urojc discussion.
Twitter is very much about ‘immediacy’ – it enabled the discussion of a key paper at short notice. This type of post publication ‘peer review’ with such immediacy was unheard of until now – proudly, urologists are leading the way! I think it would be an excellent idea to a blog summary for those who miss the discussion – reading the transcript afterwards is always more difficult to follow compared to following the discussion as it unfolds. We should look to identify volunteers to summarise the discussion after each month’s #urojc.
Thank you Declan, Stacy and Matt and also to all who have provided feedback off line on on line via Twitter. It is clear that the #urojc is moving beyond being a pilot project and will move to become a recognised modern day urological CME option. I am keen to see it expand beyond uro-oncology topics and would be eager to hear from any volunteers who are keen to take ownership of the other areas within urology. Applications via Twitter of course!
Henry, from a trainee perspective, I think this is a great vehicle through which training urologists may not only be exposed to the latest literature (immediate indeed) but may also be challenged by opinions from internationally respected urologists.