PRECISION delivers on the PROMIS of mpMRI in early detection of prostate cancer
Today, Dr Veeru Kasi of University College London, presented the results of the PRECISION (PRostate Evaluation for Clinically Important disease: Sampling using Image-guidance Or Not?) study in the “Game Changing” Plenary session at the #EAU18 Annual Meeting in Copenhagen. The accompanying paper was simultaneously published in the New England Journal of Medicine. And it is stunning! Everyone in the packed eURO auditorium knew they were witness to a practice-changing presentation, and the swift reaction on social media around the world confirms this.
Fundamental paradigm shift in prostate cancer diagnostics, from @veerukasi @mrsprostate #EAU18 today, and @NEJM now online. What a day https://t.co/U7MW3oeCvV pic.twitter.com/MfpgpgGkgV
— Declan Murphy (@declangmurphy) March 19, 2018
PRECISION: MRI-targeted biopsy strategy leads to fewer men needing biopsy. Article with video interviews with Veeru Kasivisvanathan and Declan Murphy https://t.co/QXaWZLaBvo
— European Association of Urology (EAU) (@Uroweb) March 19, 2018
Congratulations to Veeru (a second year urology resident in London), senior author Dr Caroline Moore, Prof Mark Emberton, and all the collaborators on this multicenter international trial. I had the great privilege to be the Discussant in the Plenary session so have been digesting this study in detail for the past few weeks.
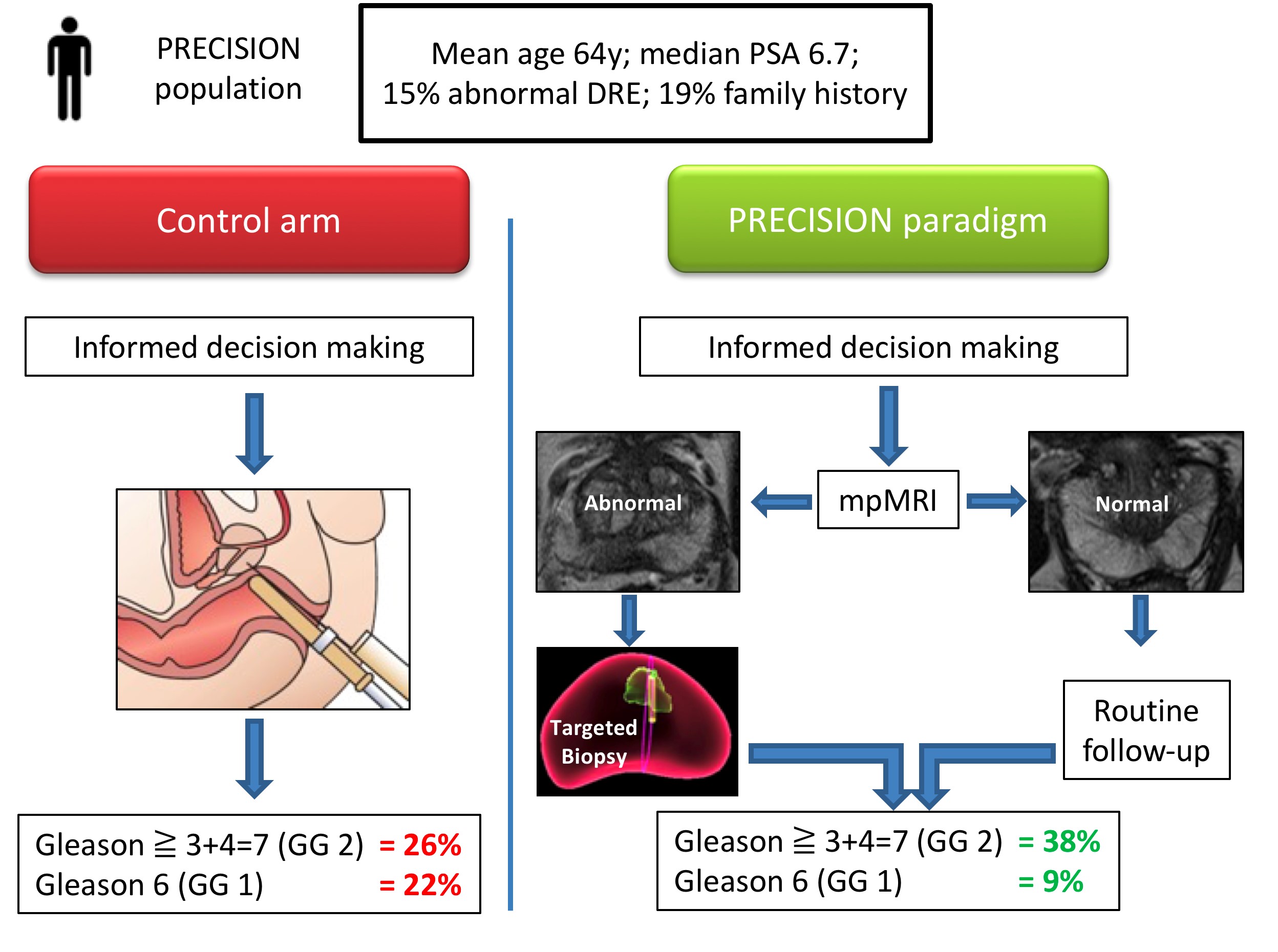
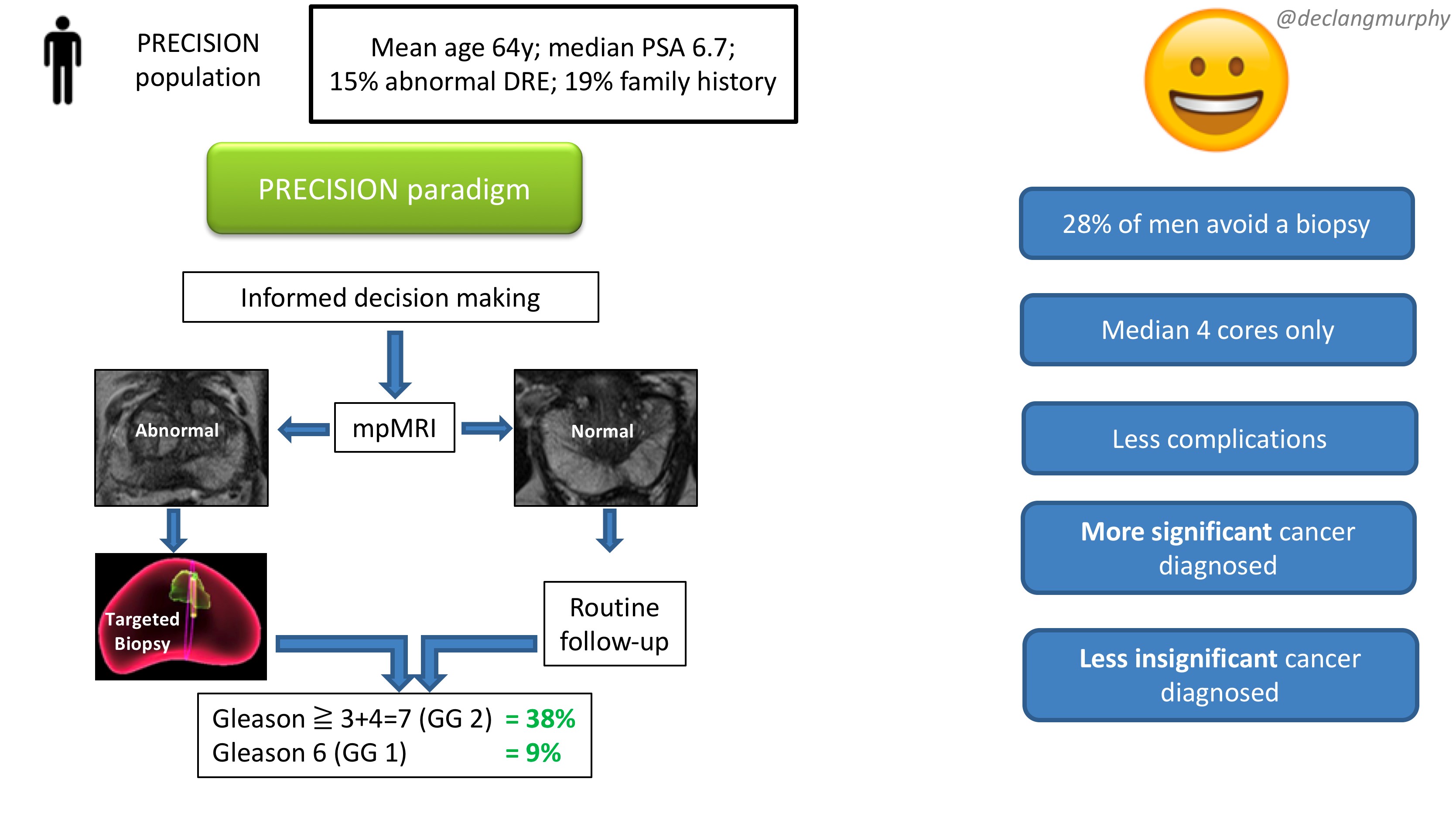
Let me summarise the PRECISION study in brief. In this multicenter international study, 500 men with a suspicion of prostate cancer (mean age 64, median PSA 6.7), were randomised to receive a standard of care (SOC) diagnostic pathway (12 core TRUS biopsy), or an MRI directed pathway. In the MRI pathway, all patients had an MRI, and if the MRI was abnormal (72% of men), they had a targeted biopsy of the lesion(s) (with no systematic biopsy; ie only the abnormal lesion was biopsied). If the MRI was normal (28% of men), they did not have a biopsy, and continued on routine PSA surveillance. The primary outcome was detection rate of clinically significant cancer; and secondary outcomes included the detection rate of clinically insignificant cancer. In the standard of care arm, the detection rate of clinically significant cancer was 26%, and the detection rate of clinically insignificant cancer was 22%. In the MRI pathway, the detection rate of clinically significant cancer was 38%, and the detection rate of taking insignificant cancer was 9%. This is depicted below in one of my summary slides from the plenary discussion.
 Therefore, despite the fact that over one quarter of men in the MRI pathway actually avoided a biopsy, the detection rate of clinically significant cancer was much greater in this arm (ie UNDER-diagnosis was reduced). Furthermore, the detection rate of the clinically insignificant cancer was much less (ie OVER-diagnosis was reduced). And all this with a median number of biopsy cores of only four, compared with 12 in the SOC arm. The reduction in core numbers along that too much less complications for these patients.
Therefore, despite the fact that over one quarter of men in the MRI pathway actually avoided a biopsy, the detection rate of clinically significant cancer was much greater in this arm (ie UNDER-diagnosis was reduced). Furthermore, the detection rate of the clinically insignificant cancer was much less (ie OVER-diagnosis was reduced). And all this with a median number of biopsy cores of only four, compared with 12 in the SOC arm. The reduction in core numbers along that too much less complications for these patients.
This looks like WIN-WIN all round!
And I truly believe that these findings should provoke an immediate change in our diagnostic pathway for early prostate cancer in two ways:
- All patients with a clinical suspicion of prostate cancer should be offered an MRI as part of their informed/shared decision making pathway
- All patients with an abnormality on their MRI scan should be offered be targeted biopsy alone.
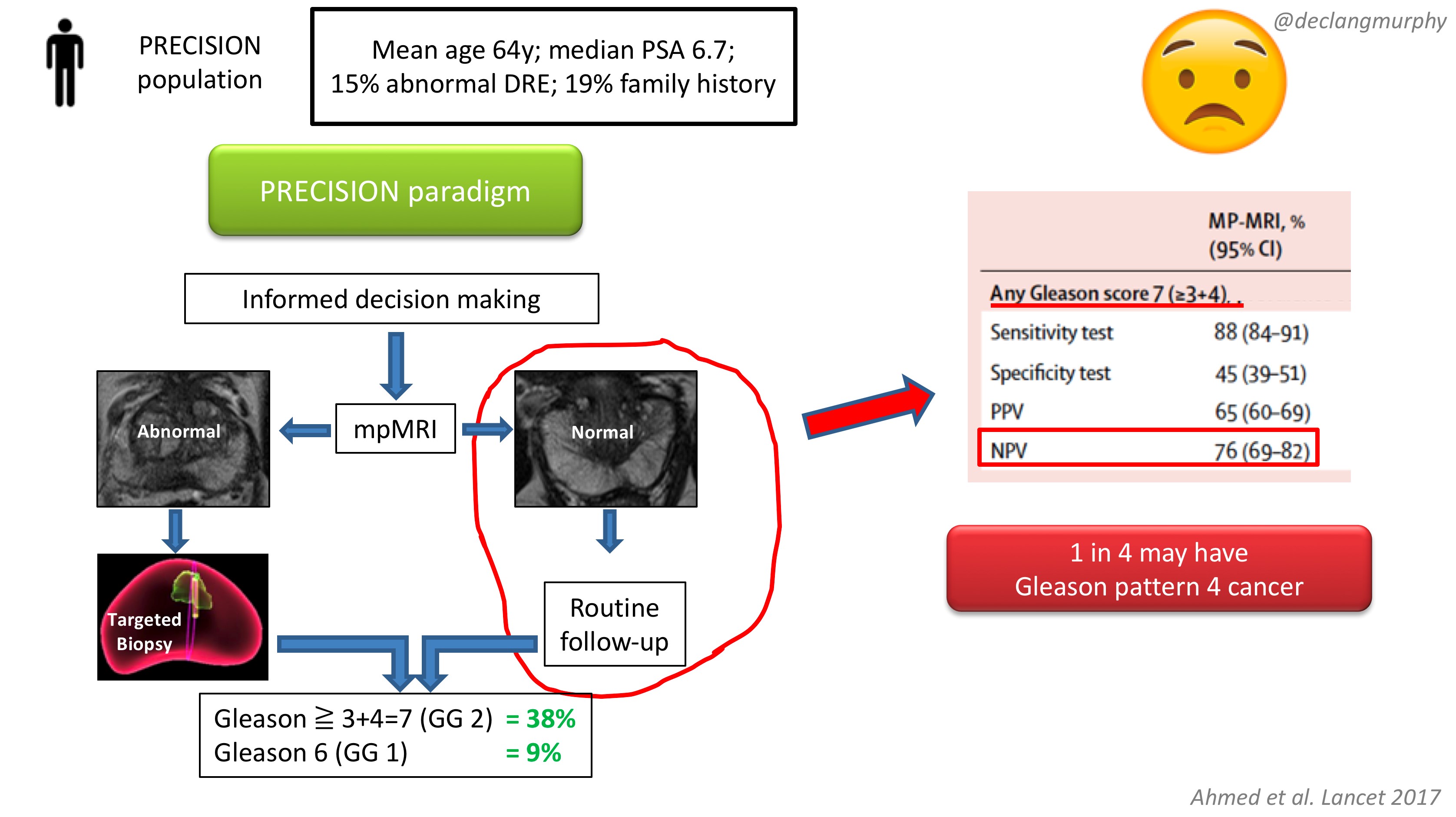
The obvious concern of course, is the fate of those patients with a normal MRI (28% of patients), who despite a clinical suspicion of prostate cancer, did not have a biopsy. How many clinically significant cancers might we miss by not offering biopsy to those patients? Of course, we already have an idea of what we would find, as the PROMIS study also included extensive biopsy (transperienal mapping) for patients with a normal MRI.
In PROMIS, the negative predictive value of MRI for detecting any pattern 4 cancer is 76% ie up to 1 in 4 men will have some pattern 4 cancer on transperineal biopsy. However, no primary pattern 4 cancers were missed on MRI. This is something we have to digest. I think that we can accept missing some pattern 4 cancers in some men, provided the “routine follow up” is adequate. But we must also continue to use the other tools we have in our multivariable approach to early detection, and if there are red flags due to family history, palpable nodules, adverse PSA parameters (including PSA density), BRCA mutations, then there will clearly be a role for systematic biopsy in some of these men with normal MRI scans.
In my opinion, we now have enough evidence to fully embrace mpMRI in our approach to early detection of prostate cancer. Following on from the PROMIS study, published in the Lancet 2017, the PRECISION study provides us with the imprimatur to fully embed MRI in the assessment of men with a suspicion of prostate cancer. The era of blind random prostate biopsy is surely over, except perhaps in those patients in whom MRI is contra-indicated. The next challenge will be to create enough capacity and expertise to make this paradigm available to all.
Resourcing will inevitably be an issue, but the PROMIS and PRECISION papers provide a compelling health economic argument for funders. Less men undergoing biopsy; less biopsy cores; less complications; less insignificant cancer – this surely makes economic sense. In Australia, where MRI has already been enthusiastically embraced, a high-quality mpMRI on a 3T machine costs $USD300, and costs are usually borne by patients. In the USA, we hear that a 1.5T MRI (with an endorectal coil) can cost USD$2-3000!! Why is this?! Australia is an expensive country – an iPhone or a da Vinci robot costs 1.5 times the cost in the USA; why therefore should an MRI cost so much in the USA? A symptom of a much broader issue with the bloated US health economy, and likely a barrier to adoption of the paradigm proposed by PRECISION.
So there you have it. A truly practice-changing study. While there will be much discussion about the nuances, I for one will immediately embrace this paradigm:
- MRI for all (I already do this)
- Targeted biopsy alone for those with MRI lesions (a new departure for me)
- No biopsy for those with normal MRI scans (unless there are other red flags).
My concluding slide from the plenary discussion:
Congrats again Veeru, Caroline, Mark and colleagues for publishing this landmark study.
Declan G Murphy
Urologist & Director of Genitourinary Oncology, Peter MacCallum Cancer Centre, Melbourne, Australia
Twitter: @declangmurphy




Wonderful summary Declan.
The Precision study now provides the RCT evidence for what is already common place practice in Australia. On the back of the Pokorny study, an Australian (Brisbane) study, published in European Urology and our own clinical experience from having ubiquitous access to high quality and affordable 3T mpMRI, it is pleasing to see that our clinical practice intuition has now been confirmed.
I completely agree with you that this study should herald a change in clinical practice.
The only worrying thing might be that 24% of patients with a normal MRI will have a pattern 4 (PROMIS data) and are not being diagnosed nor treated. Would love to see follow-up data of these men, as it might turn out missing these MRI-obscure patterns 4 are not clinically as relevant as MRI-detected pattern 4. Any data on that?
Thanks Piet – it is true that some men with a negative MRI will have some MRI-obscure cancer. In PROMIS, there was no missed primary Gleason 4 cancer, but 38 men had Gleason 3 + 4 cancer that was missed on MRI (38/308 with a negative MRI = 12%), and it may well be similar for PRECISION. The fact that more cancers were detected in the MRI-arm in PRECISION, and that baseline characteristics were similar in each arm, suggests that we might assume a greater proportion of cancers were missed in the TRUS biopsy arm.
Men in PRECISION have been consented for follow up, and this will include men who tested negative in both the MRI and the TRUS-biopsy arms. Additional testing after a negative test in either arm of the protocol was determined by usual care at that centre. We reported that 38 men had an MRI after a negative TRUS whilst 3 men with a negative MRI had a subsequent TRUS biopsy. In the TRUS biopsy arm, 3 of 9 men had a subsequent biopsy showing clinically significant cancer, whilst none had cancer detected in the MRI arm. The majority of men who tested negative in each arm were advised to have subsequent PSA testing.
It will be interesting to see if MRI-obscure pattern 4 cancer is less relevant than MRI-detected pattern 4 – something to look at in the MRI active surveillance cohorts.
Piet’s stats look correct to me. The NPV of MRI for any GS 3+4=7 disease in PROMIS is listed as 76% in the Table. 308 = the number of men with GS 3+4 on mapping biopsy in the whole population, not the number with negative mpMRI (n=158). 38 pts had GS 3+4 missed on mpMRI as per Table S7 (Appendix). So, of the 158 patients with a negative mpMRI, 38 had GS 3+4 on mapping biopsy (38/158=24%).
Terrific summary of a truly practice-changing study. And, from a practical standpoint, U.S. urologists will find this citation useful in obtaining insurance authorization to perform MRI prior to biopsy.
Declan
Well summarised. Congratulations to the authors. This study certainly does provide “food for thought”. The main restrictions as you point out will be access and costs and the real one- trusting our MR radiologists. This last point is critical as several papers in our region have demonstrated a PIRADS 3 lesion to be closer to PIRADS 4. Will this improve with time? The default of Transperineal over TRUS largely in our region is yet another nuance to be tackled. Hence this data will thus likely need to be reproduced in other jurisdictions before being completely embraced. Still it definitely makes a case for better funded MRI..
This trial is most certainly a Win-Win for those in prostate diagnostics. It avoids biopsy in almost 30% of men and diagnoses less low risk cancer whilst finding more high risk disease needing treatment.
This has huge health economic benefits in a public healthcare environment by allowing the men who really need treatment to be diagnosed early and effectively.
Many centres have been doing this approach on an ad hoc basis for the last few years but this gives us the hard evidence to put up front MRI into the frontline.
Yes we will need to follow those men not biopsied with further PSA but that is better than diagnosing lots of low risk disease.
Huge congratulations to Veeru Caroline and Mark.
Great discussion and fantastic summary Declan. The evidence for a change in management is certainly compelling, as we currently understand it. This would appear to be the future gold standard. Longer term follow-up data of the ‘normal’ mpMRI Group may be considered important for changing and implementing new guidelines.
Great summary, love the graphics. This study will drive healthcare equality in the UK – surely NICE must now recommend pre-biopsy MRI and healthboards will have to find a way to offer it : no more postcode lottery for prostate cancer diagnosis. Should be a no brainer anyway – reduced no. Biopsies! And the complications that go with. Long term follow up of mri negative men needs studied but this will come.
Great summary Declan. This pathway has been pretty common in UK since PROMIS data. Clear benefits for most men. Well done Veeru, Caroline et al, and well done EAU RF for part funding this.
Key issues will be:
1. Informed understanding by men that ‘no biopsy’ does not equal ‘no cancer’. Need to ensure patients/GPs aware of need for re-refer/re-assess should PSA keep rising, DRE change or things progress.
2. Would help to have clear pathways in men with normal MRI or normal biopsy/abnormal MRI. In ProtecT and CAP data – we saw that many men with low PSA or normal (not MRI guided) TRUSS Bx had lethal prostate cancer (see JAMA Supp figures).
3. I suspect we will all be comfortable for a few years until these Gleason 4’s present.
But in the face of the flawed random TRUSS bx and rising bacterial resistance these data clearly improve things.
Jim
There appears to be no downside. Less men needing a biopsy, less biopsies for each patient, less clinically insignificant needless diagnoses, more significant disease found- so less under sampling, possibly less biopsies will mean less biopsy complications. I started this at The Royal Marsden Hospital this morning. Booked several lesion only targeted biopsies. Until another trial of this quality says otherwise that’s what we’re doing. Thank you Team Precision!
Very nice summary Declan and congratulations to the investigators for an excellent trial. It strikes me that an even better benefit to MRI would exist if PIRADS 3 were followed instead of biopsied. This would result in an additional third of patients avoiding biopsy (initially) and would only miss 12/252 (5%) clinically significant tumours (Figure 3 in the article). Lumping the PIRADS 3 with the negative MRI could provide substantial savings and presumably the small proportion with significant cancers would be detected with follow up.
For resource strapped countries (like Canada) it would be helpful to know if there were particular subgroups that benefit the most. Were any data presented stratifying patients with normal DRE vs abnormal DRE? It would also be interesting to see the data stratified by PSA.
Many thanks again for the summary and comments.
-Rod
Congratulations to the authors on a wonderful paper , and their presentation at EAU. The pre biopsy MP MRI paradigm has been very common and almost standard of care in Australia for many years , partly due to the low cost of privately funded MRIs in our country as indicated by Declan Murphy. Like Declan, every patient I have seen for the last 4-5 years has undergone a pre-biopsy MP MRI prostate. This study does provide concrete evidence that MP MRI should be done prior to biopsy.
Whilst I also agree this study will inform governments and may assist with funding this technology for patients, as someone who has been in discussion with our Government for 3 years to get MP MRI prostate funded , health policy issues do arise. Governments/payers/hospital trusts do not want to pay for both MRI and biopsies; they will want an either/or situation . They fully understand the need to biopsy if there is an abnormal MRI but there will be strong push back from payers to fund a systematic biopsy for a normal MPMRI , even more so after PRECISION.
So are we completely confident of an either/or situation yet from PRECISION data ? I am still not quite sure . Based on PROMIS data 11% of Gleason 4+3=7 or greater cancers were missed by MP MRI on a trans-perineal mapping biopsy , and 28% if one defined a clinically significant cancer as Gleason 3+4=7 or greater . If we look at studies comparing MP MRI to whole-mount radical prostatectomy specimens 20% of index cancers were missed on MP MRI , with presentations at EAU this year once again supporting that data. We also have to take into account , the participants in PRECISION were all centres, with expert radiologists and urologists – so can this be translated into the general community at this stage ? Lastly if we are really serious about reducing complications from biopsies especially sepsis , then changing to trans-perineal biopsies is a far more effective way of reducing sepsis to virtually zero compared to reducing core numbers by TRUS biopsy , and in any case there is very limited data that reducing core numbers actually reduces septic complications.
Are we ready to abandon biopsies in all men with normal MP MRI prostate , especially those with high PSA densities, or high PHI , or change in DRE , etc.,? If we are then some ( perhaps up to 20%) of clinically significant cancers will be missed, and even higher rates of missed significant cancers from less experienced centres. 2 of our previous contributors to this blog authored a paper ” Gleason 3+4 , active surveillance no more ” so if these cancers deserve active treatment then they must be diagnosed, and not missed .
Certainly with discussions with payers we need to identify risk factors that may still raise suspicious for clinically significant cancers ( as mentioned above ) so that even with a normal MP MRI, biopsies can still take place and will be funded . It will remain a delicate and difficult conversation with payers that everyone needs to be prepared for as they go down the path of changing to a MRI based biopsy paradigm. .
At the risk of splitting hairs, Caroline Moore’s comments re GS 4+3 with negative mpMRI in PROMIS appear to be correct (i.e none were missed). The 89% NPV for the primary definition of clinically significant prostate cancer (GS 4+3 OR core length >/= 6mm) was purely due to 11% cases having core lengths >/=6mm on mapping biopsy; all were GS 3+3 or 3+4. This is shown in Table S7 (Appendix).
Jonathan , thanks for the clarification . I don’t want to be misunderstood , I am a huge fan of MRI prostate and in particular of this paper as it has validated what we have been doing in Australia for several years . My only points really were that these centres are outstanding in their radiological and urological capabilities so we do have to be careful before assuming everyone in general urological practice can achieve these outstanding results. Secondly we have to assume that some low and low intermediate risk cancers will be missed, at least for a while until they progress (as Caroline Moore has indicated in her post). I personally have no issues with this as I have been managing these patients with active surveillance for some time. Others have been very concerned about inclusion of any Gleason 3+4 in an AS program and implementation of PRECISION will mean that will occur in a small number of patients as their low intermediate risk cancers may go undiagnosed until progression, so we all have to be comfortable with that. Lastly I wanted to share my experience in dealing with payers regarding this issue. At least in Australia. the red flag patient with a normal MRI eg., young , slightly suspicious DRE , very low % free PSA, high PSAD ( as described by Caroline Moore ) etc., may potentially not have been funded for a biopsy. Whilst we are still awaiting our Government’s final decision about funding prostate MRI services, there is no doubt that they were not keen on funding any red flag biopsies if MRIs were “normal” and the urological committee advising the Government certainly had to put a strong argument forward against that decision and to ensure urologists continued to have clinical independence in the decision making regarding the need for a biopsy,.I hope we were successful but I simply wanted to bring that issue to everyone’s attention as similar battles might spring up internationally. I just want to make sure that if there are factors that make a urologist concerned , that patients are still able to access a systematic biopsy if required and clinically indicated. I totally agree with the authors that in the vast majority of cases a biopsy is not required for a PIRADS 1,2 lesion , and is even borderline with a PIRADS 3 lesion based on the PRECISION results .It is indeed a win/win for patients. Finally I do want to congratulate the authors again; it is a critically important landmark study and there is no doubt that MRI prior to biopsy is now the standard of care.
Declan, thank you for this comprehensive summary of a truly commendable study. This study will hopefully mark the end of blind random biopsies. Using MRI pre-biopsy, with MR targeted biopsies in patients with abnormal imaging only has been our eminence (= Hein Van Poppel) – based approach in UZLeuven, long before evidence of PROMIS and PRECISE was available (not something to be proud of, but was long before I came to senses during my Melbourne fellowship). I understand your worry for the 24% missed ISUP GG2 lesions in PROMIS, but many of these (small size) GG2 tumors will not need treatment or will show themselves on repeat scans if clinical suspicion continues. Nevertheless, until we have evidence for that, your systematic biopsies for those with negative MRI but red flags” should be the 2019 EAU guideline recommendation…
Fantastic to have confirmation of what a number of local audits have found. The next question is the role of MRI in active surveillance: can we reduce repeat biopsies?
Great blog … was any subgroup analysis on race or family history taken in account ? .. if a black man or man with 1st degree family history (or both) has -ve MRI should he be treated the same as non black pt and not biopsied if MRI not concerning ?
We work in a population with one of the highest percentage of African and Caribbean men in the UK (south London) .. is this study still applicable to this group ( given risk) Or should bx be offered if clinically suspected but MRI reassuring .. jury still out ?
Great paper for all urologists. 3T MRI is our go to investigation, followed by biopsy if abnormal.
Could do with some guidance from societies/EAU/AUA//USANZ/BAUS as to wheather we should JUST target biopsy or target and standard biopsy BASED on this paper.
If we’re only performing a few targets biopsies now, do we all need to go to trans-perineal or should we use TRUS biopsy!! Maybe the next paper!!!
Well done on the paper
At UCL, and many other centres, our pathway includes:
1. Positive MRI with negative biopsy needs discussion between radiologist and urologist , with histology review. Inflammation and atrophy can mimic cancer, so reassuring if present. If MRI still scored 4 or 5 after review then either repeat biopsy or 12 month MRI recommended.
2. For men with a score 1-3 and no cancer on biopsy, or no biopsy: set a personalised PSA threshold for re-referral, taking into account current PSA density, and other risk factors including age. Suggest annual PSA with GP and re-referral if PSA reaches threshold.
3. Discussion with patient re competing risks – 10% risk of missed 3+ 4, reduced to 1-2% using PSA density to select men with negative MRI for biopsy. 5mm template mapping biopsy has 20% acute urinary retention and 10-15% new ED, mostly temporary.
4. For MRI incompatible men eg pacemaker we do transperineal 12 sector biopsy .
Great summary and for those with high quality moMRI this will definitely change practice. Like you I already perform an MRI prebiopsy and don’t biopsy men with a PSA <10ng/ml and a normal scan. However it is important to emphasise that you need to be confident in the quality of the MRI and it’s reporting and an audit of local data might be wise before this is implemented everywhere
What an important study and what a terrific summary by Declan. It would be interesting to see how the current findings could be translated into a nomogram / risk calculator for prostate biopsy. Combining imaging findings with PSA / volume / stage will likely lead to even better outcomes. However, centres should be careful to switch to a MRI-dependant pathway before MRI and radiology quality are guaranteed.
Excellent summary Declan and great discussion by all.
Another strength of PRECISION was the heterogeneity in clinician involvement, being 30-40 clinicians for each of performing biopsy, interpreting MRI and pathology. To my mind this removes an “expertise” bias (of centralised, single centre, high volume studies) and, with similar results to those from experts, is more applicable for urologists outside the study – a “real world” study design.
The approach to biopsy will require some further refinement in future studies. ~90% underwent transrectal approach for the MRI-GB (resulting in more UTI, 2.4 v 1%; same sepsis/prostatitis rate) and >80% used software-assistance. With motions away from transrectal/transfaecal route (to transperineal, likely more expensive) and a high dependence on software-assistance, will the overall cost of a biopsy when required be much higher than current? Hopefully the less overall biopsies offsets this enough, or with more practice, equivalent cognitive approaches will be the main stay as shown by several studies.
Outstanding papers (including PROMIS) and collaborative effort, truly practice changing.
Thanks Caroline. For a long time there have been few urologists that would have had a prostate biopsy without a prior mpMRI, so PRECISION along with PROMIS proves that expert opinion is often correct. There are probably still some urologists that won’t have their PSA measured although with these studies the fear of unnecessary biopsy or treatment must be reduced.
The next question for me is whether we would all have an mpMRI on the basis of a single PSA that is mildly elevated, or forego a biopsy if the PSA keeps rising or PSAD is high.
At least here in Scotland we are short of radiologists in general, and the number of expert mpMRI reviewers is small so it seems to me that a reliable point of care test(s) that allow even better risk stratification and select those who require further assessment immediately is needed.
Declan, fantastic summary as always!
Huge congrats to the authors.
As you crystallize in the Blog, the deliverables of mpMRI / fusion technology are 2-fold:
DELIVERABLE #1: Reduce harms of PSA-screening by dropping the rates of OVER-diagnosis of indolent disease (PRECISION delivers this by avoiding bx in some 28% of men and avoiding the 12-core template in those who get biopsy) .
DELIVERABLE #2: Reduce UNDER-diagnosis of high risks disease in cohorts with prolonged life-expectancy (Fusion to an mpMRI target clearly allows for a “better” biopsy).
With data from trials like PRECISION we are getting closer to locking down both #1 and #2; however, I am curious to see if dropping the 12-core template at time of targeted biopsy will readily gain clinical traction (indeed, this is the only way to achieve DELIVERABLE #1!)
In our recent pub in J Urol, we defined the concept of a Reduction Metric (ReM) as the proportion of men in whom 12-core template could have been omitted without consequence: https://www.jurology.com/article/S0022-5347(17)77673-2/fulltext
Dovetailing with PRECISION data, published series to date demonstrate that ReM ranges from 78% to 95%. Stated differently, 5-22% of men who undergo fusion targeting with 12-core template would have significant CaP missed if 12-core template was omitted.
How to handle this reality in clinical practice? To use your words, this we still “need to digest.” In my experience, a ~20% chance of missing significant cancer and the risk of OVER-diagnosis of indolent disease is difficult for most patients to balance.
In the meantime, U.S. based insurers like Aetna and Cigna need to face these data from PRECISION and PROMIS and begin approving reimbursement of mpMRI for men who presents with elevated PSA and are biopsy-naive. Unfortunately, currently reimbursement for such patients from these payers is largely non-existent.
What a great blog and discussion about a wonderful paper; for me, akin to a personal tutorial on prostate diagnostics. A masterclass.
So much to think about – Piet Ost “do mri visible / invisible tumours carry the same risk ?”; Jon Mak “same in black men?” and Mark frydenberg “payers want an either/or not both in everyone”
2 thoughts:
1. Does a surgeon need to know what’s going on in the non target areas of the prostate to plan the Tx/ radical prostatectomy ? ( Ps I don’t do them !)
2. Does a more comprehensive biopsy strategy eg TP sector post mri (not mapping) , allow a
patient to be discharged not followed up “ no more psa, no more mri, no more visits. Move
on …”
Thanks Tim.
In response to point 1.
MRI does miss some significant T2 tumours. Unlikely to miss significant T3 tumours. If we get a positive margin on an unsuspecting T2 tumour we were in the Prostate and shouldn’t have been. That’s the surgeons fault and not the MRI!
Point 2. Good point.
Tim — here are some important data to help answer Poet Ost’s question:
https://www.ncbi.nlm.nih.gov/m/pubmed/28163032/ —> cribiform pattern tumors are more easily missed on mpMRI. definitely an opportunity for deeper understanding of this fact…
Congratulations friends!!
The conversations on Twitter are still ongoing.
It is useful for a surgeon to know what is happening on the “normal side” as far as the degree of nerve sparing is concerned. The Scandinavian RCT failed to reduce positive margins based on MRI mainly because of margins in unexpected areas.
I am looking forward to the NICE Guidance on Prostate Cancer next year in the BJUI – not biased at all!!!
This important paper just published online in European Urology gives some insight into the fate of negative MRI patients when followed longitudinally.
n=1255 men with negative MRI, 7 year follow up. 5% likelihood of being diagnosed with clinically significant cancer at 2yrs.
Paper here https://www.europeanurology.com/article/S0302-2838(18)30183-0/fulltext
Declan, magnificent summary!
I think it a foregone conclusion that MRI guided biopsies are superior to blind TRUS biopsies. But we can make it better by adding systematic biopsies, rather than just a targeted only approach.
We know that 15% of significant prostate cancers are “MRI invisible”, there can be significant inter-reader variability in MRI reading ( In PROMIS, there was quality control in term of radiologist expertise, and not all centres made it despite training provided); and “actually hitting the target” is not perfect – there can be errors in registration.
This approach will yield the following advantages:
1) In the positive cases – knowing whats happening on the opposite side is important in terms of nerve sparing
2) In negative cases, we will be more confident that it is truly negative vs worrying about whether we are missing a MRI invisible tumour
A great discussion. Thanks Declan, Veeru, Caroline et al.
Exciting to see the new approach to prostate cancer diagnosis firming up.
As a new recruit to Freddie Hamdy’s team in Oxford, it’s been great being involved with turning around how we do the prostate cancer pathway here.
We have the good fortune to have had up-front MRI since 2015. However, until now, every patient has proceeded to transrectal biopsy based on the PSA regardless of MRI findings. Surprising perhaps, but a real opportunity as we have a unique dataset to answer a question raised in varying ways by several contributors above:
“How many clinically significant tumours (grade group >1) would be missed in STANDARD CLINICAL PRACTICE (outside of super-centre trials) if men with negative MP-MRI (PI-RADS <3) and PSAD<0.15ng/ml/cc don't get biopsied?"
The answer from Oxford with n=792 is 15%.
[Presented by Cate Hobbs and Richard Bryant at #EAU18]
Having this information from our own unit with our own radiologists has been tremendously useful as we can now accurately inform patients of the risk if they choose not to proceed to biopsy (as many do). I realise that not every unit will have had this hybrid phase with MRI that we have had at Oxford, but it is clearly very helpful for units to audit their own performance, especially give that future management decisions will firmly rest on’your risk of clinically significant disease’ discussions with our patients.
Currently we still offer transrectal biopsies to all men who do proceed to biopsy, but we are transitioning to transperineal biopsy in the clinic (Precision Point, under LA) so that we can make sure that those who do get biopsied have it done properly and safely, without crippling our theatre capacity. Personally, I still think some systematic biopsies are needed (our preferred approach is #Ginsburg_Protocol) until we understand better the interplay between imaging and the clonal genetics of prostate cancer development – but that’s a whole ‘nother discussion. And yes, Tim, I do think it’s tremendously helpful to have the full TP biopsy sector results for planning RARP nerve sparing, bladder neck and apical dissection.
Also, the #proststeJC 48hr journal club will feature this paper starting Mon 26th March at 10am ET. Follow @PCF_Science for details
If we only need focal diagnosis, does that mean we also only need focal therapy ?
We have developed the following draft pathway at the NHS England Cancer Communities of Practice, in order to reach agreement on a pathway suitable for widespread adoption in the English NHS, where many centres already use pre-biopsy MRI. This is especially so for men on a ‘timed pathway’, where fines can be incurred if referral to diagnosis exceeds 31 days, or referral to treatment exceeds 62 days (strange concept to those working in other countries!!)
Great input from groups all around the country including the Vanguard partners (in particular Satish Maddineni & Noel Clarke at the Manchester Cancer Collaborative, myself and John Hines at the UCLH Cancer Collaborative, and Hash Ahmed and David Hrouda at Royal Marsden Partners), as well as many urologists, radiologists, mangers and patients from the alliances around the country.
Great blog Declan. One of the massive advantages of MRI driven biopsies is the dramatic reduction in diagnosis of tiny foci of 3+3=6 small volume low risk cancers that fill up our follow-up clinics with active surveillance patients. No question that this is the way forward.
Declan — fabulous summary! A beautifully written piece summarizing the findings of PRECISION, tying in the results of PROMIS, and highlighting several of the factors/challenges of making this new standard of care a pragmatic reality.
Two personal thoughts, that you have already hit on:
1) The men with a negative MRI who harbour pattern 4 disease: As you mention, red-flags will prompt systematic biopsy. For those without red flags, when and how often to intervene downstream will need to be fleshed out (repeat MRI? systematic biopsy? biomarkers?).
2) Economic challenges: this trial is truly practice changing, and it is very difficult to argue with the science presented (and I certainly am not). As someone starting a staff position in an economically challenged region of the US in a few short months (Medicaid, uninsured, poor SES status, etc), I know I will be unable to offer an MRI prior to biopsy for a cohort of my patients. But, as clinicians, it is our job to (i) conduct high quality studies that push policy makers to make changes (as you’ve mentioned herein), and (ii) continue to be champions of standard of care for our patients.
Congrats to the investigators for conducting this trial, and again to you Declan for the blog post and Discussant presentation at EAU!
Great paper and terrific summary @declangmurphy!!! By the way fantastic comments above and also, thanks Caroline Moore for sharing with us your pathway on NHS.
I was pretty lucky to be in Australia as a fellow in 2016-2017 and I can tell you that we were already doing MRI for a great number of patients even before the first biopsy. Mainly , we were utilizing that also for clinical decision between a transperineal approach (apex or anterior lesion) or trus biopsy.
Fantastic to have now the confirmation that MRI before the first help us to have more clinically significant PCa and a smaller proportion of men with clinically insignificant cancer.
Really happy to live this MRI/PSMA PET/ROBOTIC “era” and even happier I was in australia to live these moments intensely.
Congratulations to all involved in the paper !
Trying (hard) to put this into daily pratice in Brazil.