Editorial: The Prostate – The gateway to men’s health
We have been told for many years that the management of men with LUTS due to BPH was, for most, about treating the impact of those symptoms on their quality of life. However, evidence has been accumulating over recent years to suggest that BPH may be associated with the various components of the metabolic syndrome – a combination of central obesity, impairment of glucose tolerance, dyslipidaemia and hypertension. Hammarsten et al. [1] examined the link between BPH and 22 individual aspects of the metabolic syndrome and found that BPH was linked to 21 of these factors, including increased body mass index (BMI) and waist circumference, hypertension, type 2 diabetes, dyslipidaemia and atherosclerosis, lending support to the hypothesised association with metabolic syndrome as a whole.
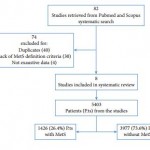
In this issue of BJUI, Gacci et al. [2] report the results of a meta-analysis of eight studies examining this link between BPH and metabolic syndrome, including >5000 patients, of which over a quarter had metabolic syndrome. They report a higher prostate volume (and transitional zone volume) in men with metabolic syndrome than in those without, particularly in older and obese patients and those with low high-density lipoprotein (HDL)-cholesterol levels. Interestingly however, no difference was seen between the groups in terms of LUTS, as measured by total IPSS or the storage/voiding sub-scores, although other studies have reported this in the past [1]. They conclude that modification of lifestyle and cardiovascular risk factors, by weight loss, increased exercise, dietary improvements etc., may have a role to play in improving LUTS. In addition, further exploration of the role of medication, such as statins, in the management of LUTS due to BPH is recommended. These conclusions are supported in the literature by observational studies, showing for instance a decrease in the severity of LUTS with increasing exercise, an increased risk of LUTS with obesity, and a delay in the onset of LUTS for patients taking long-term statins of up to 7 years [3, 4].
BPH is not the only urological condition that appears to have links with metabolic syndrome [1]. It is well established that erectile dysfunction has strong associations with type 2 diabetes mellitus, cardiovascular disease, obesity and sedentary lifestyle. Less well known links are also seen with prostate cancer, renal calculi, hypogonadism and overactive bladder [5]. We are familiar with carrying out cardiovascular risk assessment, screening for diabetes and giving lifestyle advice to men with erectile dysfunction. Given the evidence suggesting that erectile dysfunction and BPH are closely associated, with many men suffering from both conditions [6], it would suggest that perhaps we should be doing the same for men presenting with symptomatic BPH.
An awareness and understanding of the connection between BPH and metabolic syndrome should encourage all physicians to assess patients with LUTS/BPH for underlying cardiovascular risk. It suggests that as a minimum, a number of baseline investigations should be carried out: blood pressure measurement, a fasting lipid profile (and formal cardiovascular risk profile using established algorithms, such as QRISK®), assessment for diabetes using fasting glucose or glycated haemoglobin (HbA1c), measurement of weight and BMI, or ideally the measurement of abdominal circumference (as central obesity is a far more sensitive marker of risk than BMI). Identification of features of the metabolic syndrome allows for tailored lifestyle intervention, in terms of increasing exercise, dietary changes, weight loss, smoking cessation advice and alcohol moderation. Medical management of hypertension, diabetes, dyslipidaemia and cardiovascular disease may be required according to national guidelines.
Huge numbers of men die prematurely from cardiovascular disease and complications of type 2 diabetes, and men are renowned for poor engagement with primary preventive strategies to decrease this risk. Men presenting to their GP or Urologist with symptoms from BPH are therefore presenting us with an opportunity to intervene and potentially save lives in the process – the prostate can be considered a gateway to wider aspects of men’s health, far beyond the quality-of-life impact of LUTS.
Jonathan Rees
Backwell & Nailsea Medical Group, North Somerset, UK
References
1 Hammarsten J, Peeker R. Urological aspects of the metabolic syndrome. Nat Rev Urol 2011; 8: 483–94
2 Gacci M, Corona G, Vignozzi L et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int 2015; 115: 24–31
3 Parsons JK, Messer K, White M et al. Obesity increases and physical activity decreases lower urinary tract symptom risk in older men: the Osteoporotic Fractures in Men Study. Eur Urol 2011; 60: 1173–80
4 St Sauver J, Jacobsen SJ, Jacobson DJ et al. Statin use and decreased risk of benign prostatic enlargement and lower urinary tract symptoms. BJU Int 2011; 107: 443–50
5 Rees J, Kirby M. Metabolic syndrome and common urological conditions: looking beyond the obvious. Trends in Urology and Men’s Health 2014; 5: 9–14
6 Rosen R, Altwein J, Boyle P et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 2003; 44: 637–49