Editorial: Sergeant, do you copy?
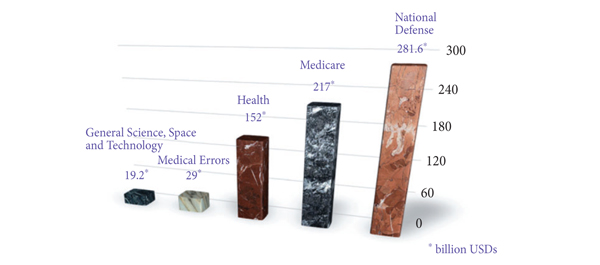
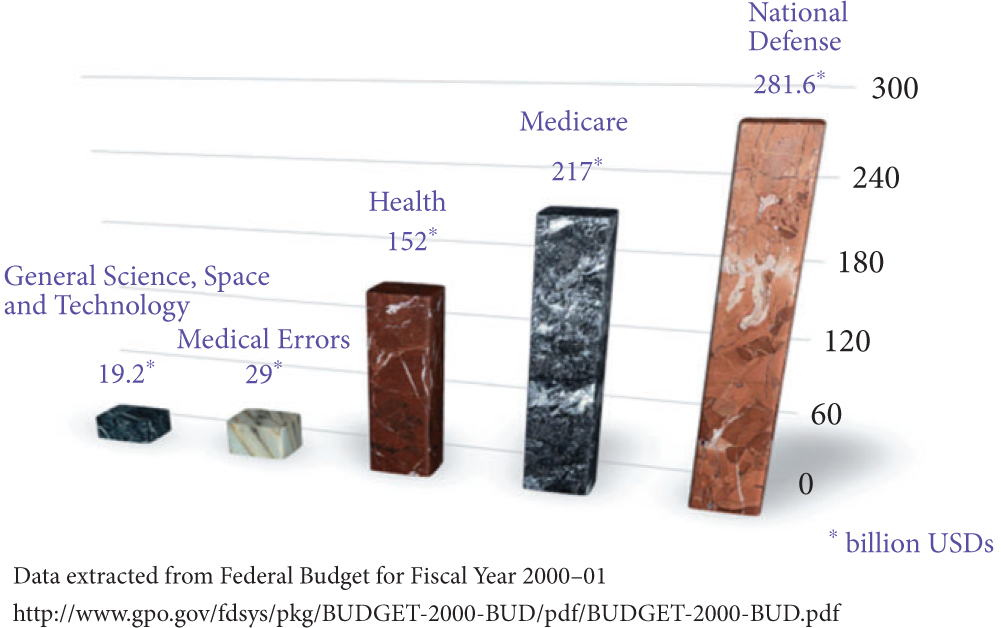
In the Institute of Medicine report published in 1999, it was estimated that 44 000–98 000 patients died annually from preventable medical errors. It was further reported that the annual burden on economy due to preventable medical errors was anywhere between 17–29 billion American dollars. In the USA federal budget 2000–2001, the entire federal resources devoted to general science, space and technology was 19.2 billion American dollars: ≈10 billion less than the cost of medical errors (Fig. 1).
Figure 1. The magnitude of problem caused by medical errors. USDs, American dollars.
On root cause analysis of the errors identified in the Joint Commission on Accreditation and Certification database (2011), it was reported that most of these errors are non-technical, i.e. human factors (72%), leadership (65%), communication breakdown (61%), etc. Furthermore, Greenberg et al. studied the patterns of communication breakdown on the Malpractice Insurers’ Medical Error Prevention Study (MIMEPS) database and concluded that breakdown patterns were similar preoperatively (38%), intraoperatively (30%) and postoperatively (32%). Most errors were due to miscommunication within a single department (78%), as compared with across departments (19%) or institutions (3%). In 49% of the cases, the information was never relayed and in 44% the information relayed was not comprehended appropriately. In all, 29% of these errors involved a surgery attending at transmitting end and 56% at the receiving end of information. In all, 85% of these communications were verbal.
In this issue of BJUI, Ahmed et al. have used the Healthcare Failure Mode and Effect Analysis (HFMEA) model to design a safety checklist specifically for robotic procedures. Checklists have been heavily used in high-risk environments that involve complex technology, e.g. aerospace and nuclear engineering. Robotic surgery is another such high-risk environment, where intraoperative communication is critical. When a surgeon performs a robotic surgery, (s)he is not standing next to the patient (and occasionally not even in the same room!) and relies heavily on his/her assistant. Additionally, the bulky robot takes most of the space around the patient. Small movements of the instruments can cause abrupt and exaggerated movements of the robotic arms, which might injure the bedside assistant, anaesthesiologist, or the patient himself. Last, but not the least, there is a memory clutch on the robotic arms, and its purpose is to ‘remember’ the position of the arms while exchanging the instruments. However, if this clutch is pressed by mistake, all memory is lost and careless insertion of an instrument at this time, making an assumption of memory, can be dangerous and can cause serious injury. The safety checklist described by Ahmed et al. is one of the first checklists specific to robotic surgery. In parallel to this, the Fundamentals of Robotic Surgery (FRS) inter-disciplinary consortium led by Dr Richard Satava has also developed a checklist, specifically for robotic surgery. It will be interesting to study the actual impact of these checklists on prevention of medical errors in robotic surgery. Similar checklists have been validated showing significant clinical correlation using in situ simulation for obstetric emergencies.
Although checklists do help to a certain extent to prevent serious errors, the basics of communications must not be forgotten while communicating to a colleague about patient care. There should be no ambiguity about who is the ‘transmitter’ and who is the ‘receiver’ of information. Both the ‘transmitter’ and ‘receiver’ should have a shared mental model about the purpose of communication (‘transmitter’ is seeking guidance, giving orders, asking for an opinion, referring a case, etc.). Finally, closed-loop communication should be a part of protocol where both the ‘receiver’ and ‘transmitter’ acknowledge the receipt of information, e.g.
Console Surgeon: ‘Please replace the scissors in the right arm with the needle driver’.
Assistant: ‘OK, I am replacing the scissors in your right arm with a needle driver’.
Console Surgeon: ‘Go ahead’.
Assistant: ‘Needle driver coming in’.
Console Surgeon: ‘Perfect. Thank you’.
Sanket Chauhan and Robert M. Sweet
Department of Urology, University of Minnesota Medical School, Minneapolis, MN, USA


Very nice work from the group at Guy’s. Surgical safety has been a major focus at MD Anderson in the past 2 years and a tough culture to change. Many of the changes were spurred from our Joint Commission inspections, and our checklists come in several formats, but none specific for robotics. I believe we cover most all bases listed (not sure anyone checks off that the robot is locked, but we have a small pool of equipment techs that do this and call it out). The one part of your study the I believe needs more work involves any equipment problems encountered during the case. Equipment problems from the robot can range from disposable instruments failing too early, sterile adaptors failing, or legitimate hardware problems related to the arm movements or vision. So the problem is that if a surgeon has a problem on Monday, the next team to use the system on Tuesday may or may not be aware of the prior problem, or what was done about it. After >1700 cases, I still run into new problems here and there–recently the touch pad on the Si console failed and started randomly changing user profiles and failing to respond to touch without a full re-boot. So I learned how to get out of that jam, but we have >25 other credentialed surgeons who need to know how to recognize all equipment problems and know range of options to complete the case safely. Rather than each surgeon suffering the learning curve of equipment troubleshooting, I envision a sort of feedback loop where all users become aware of robot equipment problems as they occur to anyone and not just themselves and there is an educational component available.
Again–great contribution.
Great checklist. I recently published another one for long surgeries.
Different teams need different checklists based on experience, but there should be a fundamental core of safety maneuvers. The change in culture is one that I have commonly discovered as an issue.