Editorial: Pushing the robot-assisted prostatectomy envelope – to the safety limits? Better outcomes
The present article by Lim et al. [1] describing the new technique for robot-assisted radical prostatectomy is provocative. It really does highlight the dramatic improvement in outcomes of prostate cancer surgery for men over the last 25 years. What used to be a 3-week hospital stay with a 50% incontinence rate and a 100% impotence rate [2, 3] now becomes a day case with a high likelihood of excellent urinary control early after surgery and a fair potential for potency preservation. Twenty-five years ago men who underwent radical prostatectomy were truly brave patients.
Lim et al. report a single series by the senior author of 50 cases performed using the so-called Retzius preservation technique. Their cohort of 50 patients treated this way was compared with a retrospective cohort of the surgeon’s patients. The patients had lower-risk disease and patients who had seminal vesicle invasion or extracapsular extension noted preoperatively, presumably on MRI, were excluded from the series. The authors report a shorter operating time and an earlier return to urinary continence in the first 6 months after surgery.
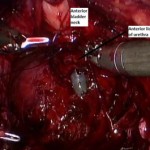
I guess where surgeons are now taking us is to an attempt to remove the prostate from the hammock of neurovascular, muscular and fascial tissue surrounding it, without disturbing the anatomy [4]. If this can be achieved then radical prostatectomy with minimal morbidity is a very compelling choice for the primary treatment of prostate cancer.
The authors’ hypothesis is that preservation of the levator fascia, puboprostatic ligaments and detrusor apron will fix the bladder somewhat like a sling would, with support at the bladder neck during increased intra-abdominal pressure.
It should be noted, however, that the present paper represents a single series of patients selected after a long learning curve by a very experienced surgeon. These excellent outcomes may simply reflect the fact that the surgeon is now extremely technically capable. It is contentious to assume that a propensity score matching of a retrospective cohort would represent a true comparator to contemporary outcomes. These excellent outcomes probably reflect technical improvements achievable with more risky and innovative surgery – after many cases. The authors should be congratulated on pushing the envelope to achieve even better outcomes for patients undergoing this operation, but the exclusion of patients with high-risk disease is probably the major negative aspect of their report. It has become increasingly obvious that patients with high-risk disease are those who benefit most from radical prostatectomy surgery. Surgery for patients with very-low-risk disease (Gleason 6) is probably unnecessary. Nevertheless, with continued insights such as those provided by these surgeons, we may be able to increase the range of patients to whom Retzius-sparing surgery in higher risk cohorts can be offered.
Anthony J. Costello
Department of Urology, Royal Melbourne Hospital, Parkville, Victoria, Australia
References
- Lim SK, Kim KH, Shin T-Y et al. Retzius-sparing Robot-assisted Laparoscopic Radical Prostatectomy – combining the best of retropubic and perineal approaches. BJU Int 2014; 114: 236–244
-
Wein AJ, Kavousi LR, Novick AC, Partin AW, Peters CA. Campbell-Walsh Urology, 10th edn. Saint Louis, MO: Saunders, 2011: 5688
-
Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. J Urol 1999; 162: 433–438
- Costello AJ, Brooks M, Cole OJ. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int 2004; 94: 1071–1076