Editorial: Does inflammation reduce the risk of prostate cancer?
Chronic inflammation is thought to play an aetiological role in tumorigenesis in several cancers including bladder, oesophagus and liver [1]. Molecular studies show that it plays a critical role in several stages of the carcinogenic process including tumour initiation, promotion, metastases and response to therapy. However the role in prostate cancer is less clear and to date, clinical studies are inconclusive.
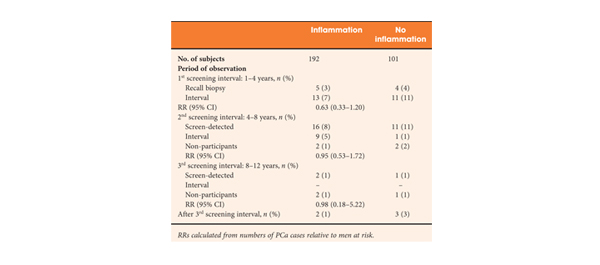
The article in this issue of BJUI by Yli-Hemminki et al. [2] appears to show an inverse association with histological inflammation and the risk of prostate cancer. Using data from the Finnish subgroup of the European Randomised Study of Prostate Cancer Screening (ERSPC) study they examined 293 patients with previous negative biopsies over a 10.5-year period and reported an 18% risk of prostate cancer in men with inflammation on initial biopsy (34 of 101 men) as opposed to 27% in those without inflammation (51 of 192 men). Perhaps somewhat surprisingly, histological inflammation did not appear to be significantly associated with PSA concentration, although it did appear that the free/total PSA ratio was higher in men with inflammation.
One potential confounding factor is that inflammation may also play a role in the pathogenesis of BPH. A large scale study showed that the odds ratio for BPH was 8.0 with a history of prostatitis [3]. Furthermore, the Medical Therapy of Prostatic Symptoms (MTOPS) study showed that men with inflammation had a significantly higher risk of BPH progression and acute urinary retention. These factors may impact on PSA levels and the chance of a subsequent prostate biopsy. However, the authors report that the inverse association of prostate cancer and inflammation did not alter when corrected for prostate volume, PSA level and age.
Significantly, those patients who screened positive at first biopsy were already excluded as were those with a suspicion of prostate cancer, such as a small atypical focus. Despite this, the study group probably represents high-risk patients, as they had all previously met the criteria for the first round of biopsies. This is borne out by the fact that the risk of prostate cancer was significantly increased when the men with inflammation on biopsy were compared with the initially screened negative men (hazard ratio 4.3). Unfortunately, we do not know what the rate of inflammation was in the control arm as they were screened negative and hence no biopsies were taken.
The significance of PSA level or prostatic intraepithelial neoplasia was not specifically investigated, although the reported rates were 32.1% and 7.5% respectively. Overall the incidence of inflammation was reported as 65%, but this included both acute and chronic inflammation. A smaller number of patients were given grade 2/3 chronic inflammation (80 and 20 patients, respectively) and only 14 patients had grade 2/3 acute, indicating most had milder degrees of inflammation. Whether this is a representative sample is not entirely clear. As the authors comment, published rates of histological inflammation do vary significantly from 8 to 99% and this does appear to vary according to detection method.
Several case-control studies and a meta-analysis [4] have shown that there is a significant increase in the relative risk of prostate cancer in men with prostatitis; however, these epidemiological studies all suffer from selection bias, in that men with clinical symptoms are more likely present and to be investigated and followed up by a Urologist. This study [2] only examines the role of histological inflammation and, at least partially, removes the selection bias associated with clinical symptoms, although it could still be argued that men with clinical prostatitis may be more likely to present for screening. This study represents a highly selected group of patients that are high risk for prostate cancer and no firm conclusions can be drawn on the general population. As inflammation is so common in prostate specimens, further high-quality large-scale studies are needed with similar long-term follow-up.
Miles A. Goldstraw and Roger S. Kirby
The Prostate Centre, London, UK
References
- Coussens LM, Werb Z. Inflammation and cancer. Nature 2002; 420: 860–867
- Yli-Hemminski T, Laurila M, Auvinen A et al. Histological inflammation and risk of subsequent prostate cancer among men with initially elevated serum prostate-specific antigen (PSA) concentration in the Finnish prostate cancer screening trial. BJU Int 2013; 112: 735–741
- Alcarez A, Hammerer P, Tubaro A, Schroder FH, Castro R. Is there evidence of a relationship between benign prostatic hyperplasia and prostate cancer? Findings of a literature review. Eur Urol 2009; 55: 864–875
- Dennis LK, Lynch CF, Torner JC. Epidemiologic association between prostatitis and prostate cancer. Urology 2002; 60: 78–83

The concept of acinar pressures might help explain how all three – inflammation/PIA, BPH, and prostate cancer could be related to one common etiology. Acinar pressures might be the mysterious source and etiology for all these lesions. Kindly refer to my Nature Reviews article to learn more. A set of brief animated videos will soon be available online to help readers visualize this concept and appreciate its potential significance in solving the many mysteries of the prostate.