Editorial: A promising solution for biofilm inhibition in the bladder, but is the application of wireless capsule cystoscopy practical?
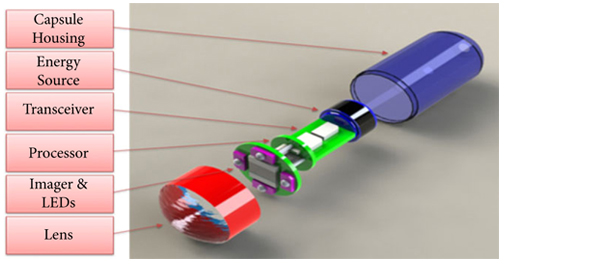
The study by Neheman et al. follows up on an idea first proposed in 2009 by Gettman and Swain to adapt wireless capsule endoscopy (WCE) technology for cystoscopy. Unlike the gastrointestinal tract where the small bowel is not endoscopically accessible making WCE appealing and advantageous, the idea of wireless capsule cystoscopy (WCC) competes with a minor procedure, office cystoscopy, that does not require anaesthesia or sedation and takes only a few minutes to perform. Furthermore, although the authors suggest that WCC would shift the labour associated with bladder cancer monitoring from practising urologists to ancillary health team providers, flexible office cystoscopy is a procedure already routinely performed by physician extenders in many offices. Nevertheless, the concept proposed by Neheman et al. is innovative and intriguing. The potential advantage of a wireless capsule cystoscope placed in the bladder safely for up to a 2-year time period, and thereby reducing the inconvenience and cost of repeated cystoscopies, could be a significant advance.
It should be emphasized that despite the title, no WCE was actually performed. The real value to the present study is the novel anti-biofilm mechanism developed that would be needed for any device implanted in the bladder for the long term. The device was housed in a semi-permeable silicone balloon filled with mineral oil that allowed a continuous slow diffusion of oil across the membrane. Based on the evidence provided in only one animal, it seems this continuous permeation of oil can interfere with surface protein adherence and consequently bacteria adhesion and biofilm creation. Certainly, this concept needs to be tested further in additional animals, aggressively exposed to bacteria, and for longer periods.
Although I am unconvinced that the concept of WCC provides significant value, the development of this biofilm inhibition technique could be pioneering. I read this study and wondered if ureteric stents and Foley catheters could be designed and impregnated with mineral oil to be released gradually. Perhaps the balloon of a Foley catheter could be redesigned and filled with mineral oil that is then released along the catheter’s entire length in a similar fashion. The true Holy Grail is the prevention of encrustation and biofilm formation on these relatively mundane devices whose chronic exchange for many patients is more costly than bladder cancer surveillance. I look forward to additional work from the authors exploring the potential of this technology.
Jeffrey A. Cadeddu
Department of Urology, University of Texas Southwestern Medical Center, Dallas, TX, USA



For those at the future of robotics Townhall at #AUA13 a reminder that the Jet Propulsion Lab from NASA believe in “swallowing the surgeon”. This is a prelude to what we might anticipate in coming years. I was excited by this article and Jeff’s editorial.