Early Prostate Cancer Detection. One Canadian Urologist’s Perspective
 After seventeen years as a practicing urologist and a further six in training, it amazes me that we still regard prostate cancer as a mystical science and view the issue of screening through the opaque prism of controversy. For so long it seems that the advanced stage disease that I learned about in the mid 1980s in medical school was irreversibly altered by early detection and treatment. Of course we now know that much of this early detection was simply a lead-time bias and that many men who were treated required only observation and were left with many potential compromises to quality of life. “Doctor, my cancer is gone, why am I so miserable?”
After seventeen years as a practicing urologist and a further six in training, it amazes me that we still regard prostate cancer as a mystical science and view the issue of screening through the opaque prism of controversy. For so long it seems that the advanced stage disease that I learned about in the mid 1980s in medical school was irreversibly altered by early detection and treatment. Of course we now know that much of this early detection was simply a lead-time bias and that many men who were treated required only observation and were left with many potential compromises to quality of life. “Doctor, my cancer is gone, why am I so miserable?”
At the recent annual meeting of the American Urological Association in San Diego, new guidelines on prostate cancer screening were unveiled. In the past, routine testing at age 50 was recommended with age 40 being the threshold for those at risk. Essentially they can be summarized as:
- Avoid screening under 40
- Do not routinely screen between 40 and 54 for average risk men. For those at risk screening should be individualized.
- For those between age 55 and 69 there is possibly some benefit and shared decision-making with a patient should be the rule.
- Finally no routine screening after 70.
- PSA should be considered every two years
The motivation for this more cautious recommendation stems for the fact that many men have indolent disease. Many of these men don’t require treatment. Treatment brings with it the potential to harm and therefore casts into doubt the value of any treatment.
The problem of course is while that may represent a possible, cost-effective strategy across the wider population, there is little doubt in my mind that this will lead to many younger and even older men falling through the cracks. It will be justified as too high a number needed to treat to make sense to find these men. Policy makers and health economists may shrug. My own experience is that we have much to learn about risk factors and that many men present seemingly without warning with significant disease.
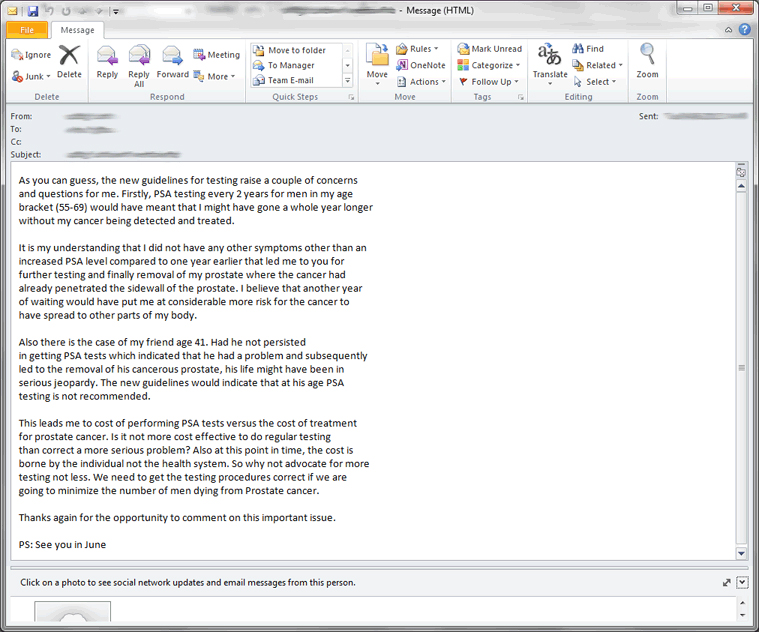
This email from a patient illustrates the concern. Identifiers of course are removed. Both men had disease beyond the capsule of the prostate. Neither man had risk factors. Our patients are very wise and quickly become experts in the disease.
In Canada, the Canadian Urological Association has taken the view for some time that we should look at multiple factors as we “build a case” for prostate biopsy. Its own guidelines reflect this. This paper that we published speaks to the use of nomograms to make better biopsy decisions. Many calculators are available on the web.
So what is shared, informed decision-making? The assumption after the AUA meeting is that somehow patients and their primary care doctors will somehow know. What sort of conversation is happening if urologists themselves don’t seem to provide clear guidance? I suspect it will go something like “PSA doesn’t work, prostate cancer is not lethal and you will likely die from something else” Many family doctors have much of their time rightfully diverted to treating important disease entities such as hypertension, depression and diabetes. A not insignificant number of primary care doctors don’t necessarily even do a DRE anymore. If the urological community conveys the message that prostate cancer is not worth the effort it will further fall down the priority list.
In my view I am a little dismayed by the rhetoric that has started since these guidelines were presented. Much of this is well intentioned and a reaction to years of potential over-treatment. This earlier 2012 piece from the highly respected @OtisBrawley of the American Cancer Society illustrates the false promise of screening message that is being told. It will only be amplified after San Diego. In my view PSA itself is a blood test. It is harmless. It is the treatment machinery that it often initiates that potentially gives it a bite and needs careful reflection.
To many, prostate cancer is simply a benign disease in aging males along the lines of male pattern baldness. This would be a disaster in my view. We have definitely shifted the curve to the left but in addition to lowering overall mortality have greatly lessened the burden of disease complications. Men presenting with hematuria, urinary retention and renal failure has significantly diminished. It is rare that we get asked to insert nephrostomy tubes for advanced disease. This was a common clinical scenario when I was a resident in the early 1990s. I think we will see much more of that if we massively abandon screening.
I think as urologists we have a big responsibility to lead within our local communities. This comment from Dr. A Partin speaks to this very well. In the absence of the perfect pre-test conditions that predict meaningful disease my view is that we have to cast a wide net. In doing so we will uncover disease that does not need to be treated. We must then be prepared to separate diagnosis from treatment and carefully counsel our patients in a way that takes much detail and effort. It is not a five-minute discussion you can have in the middle of a busy clinic. Active Surveillance does work for low-risk disease. Our patients are sophisticated and will not blindly ask for treatment out of overwhelming anxiety. In parallel, we must continue to improve. The risk of biopsy, which has greatly increased over fifteen years, must be modified. Biopsy accuracy to find “real” disease can perhaps be improved with technology such as MRI. Techniques that lessen quality of life issues need to be modified. Robotic surgery can’t be a marketing free-for-all. In other words the onus is on us experts to get it right and do better.
Prostate cancer is a very significant disease and the source of pain and suffering for men and their families. We must continue to be vigilant of its implications, respectful of patient desires and hopeful ultimately of a cure. A benign disease it most certainly is not.
Dr. Rajiv K Singal is a Urologist at Toronto East General Hospital and Assistant Professor in the Department of Surgery at the University of Toronto.
Follow him on Twitter at @DrRKSingal
Comments on this blog are now closed.




I am a person that has no knowledge of my father’s medical disposition or of my sibling.
Only due to the persistence of my general practitioner to seek another opinion, the subsequent referral to a specialist, you, your diagnoses, the operation, and the continual follow up year after year there after, have I had 10 years of a cancer free life.
Thanks
See you in June again this year.
Dr. Singal:
What a refreshing and positive article about the importance of PSA screening – finally!
As Immediate past chairman of PCCN-Toronto (formerly known as Toronto Man to Man), I along with many other survivors and support group volunteers have read the countless articles from “task forces” and a variety of “panels” which mostly discuss the potential “harms” involved in screening and tend to discourage men from even being tested. These latest guidelines from the AUA fall into this same category. What we do know is that we see and council many, many men in the 40 to 54 age bracket AFTER they have been diagnosed, and not always do they have early diagnoses with Gleason scores of 6 or 7. We also know that on too many occasions, newly-diagnosed men have told us again and again how their family physicians literally talked them out of being screened, again in many cases for years! So what different kind of “shared decision-making” will there be now with men in that 55 to 69 age group? I certainly hope that the CUA, which meets very soon, will take a very different view on the importance of screening AND of early detection.
Thank you for writing this; it is long overdue and what I wish more urologists would go on record as saying. I have yet to meet a survivor, myself included, who does not believe that the simple PSA blood test saved his life!
Take care.
Aaron. Your insight as past chairman of PCCN-Toronto is most welcome.
Certainly the profession itself has been slow embrace the concept of separating diagnosis from treatment. I do believe that most Canadian urologists share this line of thinking and I suspect as surveillance is embraced more wisely in the US the perceived harms of screening will be less. I just don’t want people to believe that not looking is fine.
In all fairness to family doctors they have to juggle a lot of things and do take their cue from us.
Very well said Aaron!
I find it interesting that testing is suggested only until age 70.
After that just let ’em die eh?
My father lived HEALTHY and HAPPY until the age of 103. But he had a prostate problem when he was around 65. Would we take away those remaining 38 good years? Yikes.
Cheers,
Eddy
Rajiv,
Thanks for sharing the new guidelines and your concern about reducing the screening regime.
My view is that doctors and labs should be required to disclose the availability of the test and it be made available at a reasonable cost. With that set in place, let the person take some accountability for the decision to test (or not).
Back to the changed guidelines, I’m interpreting ‘reduced screening’ as the same as saying fewer men will have PSA tests done. The motivation seems to boil down to the return (lives saved through early detection) doesn’t justify the money spent on PSA testing and PSA tests that result in procedures like biopsies. That this recommendation comes out of a US group (AUA), it’s not a surprise it’s a decision about the math and money.
While I’m not in a position to argue that their calculations are wrong (what $ value do they put on a life anyway?), I would recommend any male over 40 have their PSA measured tracked each year. I didn’t have any of the risk factors to warrant early screening, but did so and at age 48 my PSA score was remarkably different than the previous year. That led me to you, a DRE and decision to biopsy and then prostatectomy.
Could I have waited longer and still come out alive? Probably. Could anyone have told me exactly how long I could have waited? No. The ROI on my screening was priceless.
I wonder, if it was a requirement that men be advised when doing blood work that they could have PSA test and it would cost $20, would they? Or would they be more likely to pay $20 for an extended warranty on the big screen TV they just bought? My guess if it was required to disclose (verbally) that the test was available, many would say yes.
Peter.
PS. I doubt that there are enough urologists to handle the outcome of all men 40+ having PSA testing, but that’s a whole other issue. Be careful what you wish for Rajiv!
My turning 70 and four months later, getting a routine medical with PSA, led me to biopsy and now surgery next week. 2 years ago I had a PSA of 4/5, no family history, no symptoms and a 40 year history of episodic prostatitis. All 10 of my biopsies were positive, Gleason scores averaging 8, with 2x [7] and 2x [9]. Fortunately my CT and bone scans are negative, at this stage.
I am glad that the over 70 rule was not imposed on me!
Thanks for taking up the cause for the likes of us,
Ed Dakin
Excellent points.
It is true that many elderly men will die with, not from, prostate cancer. I would submit however that dying from prostate cancer is unpleasant and potentially unnecessary at any age.
Older men need to given informed choice. High grade disease is almost always significant
Life expectancy is much more important than chronological age. Since the benefits and harms of screening are very preference sensitive, patients in each age group should be given the evidence (including uncertainties) and the right to choose.
As discussed above, the PSA test is cheap and side effects are virtually nil. Screening is the only way to find aggressive cancers early. If the goal is to reduce overdiagnosis, we should place greater restrictions on treatment rather than screening.
Stacy is absolutely right ( and a big proponent of targeted screening). The focus must be placed on treating appropriately and not over-treating indolent disease. Still a common problem in day-to-day practice
I was 43 when I went to my family doc. I had no family history or other risk factors. I presented with night time waking to go to the washroom. My dr. Ordered a psa came back at 21 went to urologist and biopsy verified I had cancer. After surgery was told it has escaped capsule. Still had a psa after surgery and had to have radiation! If I did not have the psa test completed I may not be here today 6
Yrs after.
Thank you for the comments. Your scenario highlights the limitation of sweeping recommendations. The gate-keeping happens at the primary care level and as a profession we need to make it a clearer message
There was no history of cancer in my family on either side. So at 49 with no typical symptoms of prostate cancer, I was a little taken a back when my GP insisted he do a rectal exam during my yearly health test.
From that he recommended I do a PSA test and my life took a surreal twist… meeting Dr.Singal, the biopsy , surgery to remove the prostate and the relief to know the cancer though widespread in the organ had not breached the walls.
Had I waited a year to be officially 50, I may not have been here to write this…. 3 years clear!
Thanks!!!
I agree with Peter K who summarized it well especially his comment on the US (math and money).
Under Dr Singal’s care I have peace of mind which I gladly would pay extra if I was ever to be restricted from PSA testing because of age (73). Reading other comments, clearly the testing decisions were critical to early discovery. That is also my experience with a number of friends of all ages all of who are alive because of early testing leading to successful surgery outcome.
Rajiv,
Excellent Post!
It Brings Back Memories…
Memories of a time when, before PSA, we detected prostate cancer by DRE.
Memories of a time when my partner just didn’t feel right.
https://www.stomacloak.com/blog
Memories of when I lived in the Detroit area and watched the CBC with my wife so that we could get a different, arguably more accurate, perspective about what was going on in our own county.
Enjoyed Reading Your Perspective.
Brian
Thank Brian. The more evidence we accumulate in medicine the more the art of practicing it becomes necessary
Great comments Brian. There is much to do to get better but we cant give up the gains we have already made
I must say that I do find all of this “splitting of hairs” rather perplexing… though do understand the need from a broader socioeconomic perspective to set policy…
I realize that every patient is different so I will just offer my perspective… which is GET TESTED!! at least yearly!!… What is the cost of a DRE?… just a couple of minutes of doctor time at a regular physical?… so what is the net economic savings to the health care system by not doing them … effectively zero (maybe the physician bills the system for this??)… if the patient is asymptomatic, has a test done and has to pay for it… then the net health care savings by not doing the testing is ZERO!… thus I would conclude that not doing a DRE or a PSA test does not save the health care system anything. In fact the flipside impact of not testing can have enormous repercussions to the patient as the earlier comments have noted… by leaving the untested cancer to grow and then subsequently having to be removed in a more advanced state requiring additional treatments … thus the net actual costs to the health care system are increased by not testing… just my math…
… so why not have a policy where at each physical a family doctor explains the benefits and downsides of testing… then all of the testaphobic/DREphobic ostrich types out there can refuse the test and live the thrill of rolling the dice maybe living against the odds… and all of the prevention/detection minded folks will live the thrill of the Russian roulette testing life of hoping for a clear test each visit yet finding comfort in the proactive strategy of strike early, strike hard… then living long and prosper…
My perspective is coloured of course by my life experiences… I will self-identify as being strongly of the prevention/detection mindset and have insisted on a DRE at each annual physical since my 20’s (in spite of not having any of the “traditional risk factors”)… fortunately for me, having followed this testing regime, at age 45 my family doctor found during a routine DRE that I had a new irregularity to the shape of my prostate… even though my PSA was still like 0.8… I elected for the biopsy which showed that I had prostate cancer 😮 I volunteered to have a radical prostatectomy in the summer of 2010 and have recovered fully since… apparently our species can still live without a prostate! 😀
Just do it!!
Excellent and timely article. Many thanks to you for taking a practical stand on this critical issue. Better to work with the best that we have, understanding the limitations, than throwing the baby (and men’s lives!) out with the bath water!
And that is not to say that we shouldn’t be continuing to find new and better ways to test and to distinguish the indolent from the aggressive–far from it.
In the meantime, don’t rest…test!
Rocco
Very well said Rocco and thank you for your commitment to prostate cancer advocacy in Canada as chairman of PCCN.
Very thoughtful response Rocco. We must find better ways to screen and treat but not lose any gains we have made over the years
Rajiv,
We speak frequently about this topic and I echo your sentiments in this well-written blog. I share your frustration regarding the imperfections of current prostate screening modalities; and regarding the fact that these imperfections have seemingly led to a blase attitude toward an incredibly prevalent malignancy. I often feel that the pendulum swings too quickly in healthcare. The PSA era led to a dramatic stage migration and a significant decrease in prostate cancer deaths – clearly a good thing. We subsequently became aware of lead-time bias and the important issue of potential overtreatment, but should this justify overlooking the former?
My main concern is knowledge transfer. Even without scrutinizing the specific content (e.g. 70 years is so arbitrary – life expectancy is a more appropriate criterion) — What is the main message getting to family doctors and patients in the wake of these guidelines? “Guidelines”, by definition, are (hopefully) evidence-based statements intended to guide decision making.
Ideally, family doctors should discuss the merits and potential downsides of screening with each individual. They should convey that screening test results may lead to the recommendation of a biopsy; and that even “early-detected” prostate cancer has highly variable implications, prognoses and management options. Active surveillance for low-risk prostate cancer has surely mitigated somewhat against over-treatment and its potential morbidity.
After the USPTF statement and recent AUA guidelines, negative momentum seems to be building with respect to prostate cancer screening and it is disconcerting indeed. Risk stratification makes sense and cost effectiveness is at the crux of any widespread program. However, guidelines should not be interpreted as blanket statements that drive apathy. We need to ensure that family doctors are educated and not confused or deterred.
Ryan Groll
Urologist, Toronto East General Hospital
Ryan, thank you for your comments and for being such a great colleague. We must do better at informing family doctors otherwise it will become a forgotten disease. GPs have many, many other things to also worry about
Thanks for this post Dr. Singal. As we’ve discussed on Twitter, screening is a broad and complicated topic, but I think you’ve clarified well that the major issue with overdiagnosis of prostate cancer is the overtreatment of prostate cancer. I look forward to a time in the future when we are better able to identify which men need to undergo treatment. I expect we can reduce the number needed to treat in order to save one life, and spare more people the side effects of intervention. Additionally, while incidences of prostate cancer are relatively stable recently, mortality continues to fall – it’s likely that this is due to advances in treatment, and not just catching it earlier.
Dr. Groll’s comment is an an excellent model for an ideal discussion between a family physician and patient. I do think it adds to the original post in that it helps convey to a patient that undergoing screening is not entirely benign. The anxiety and the biopsy are side effects in themselves that we are subjecting many men to. I truly hope this conversation can happen across the country.
I am lucky to be training in the “PSA-era”, and I have had to see significantly fewer patients presenting with painful or paralyzing metastatic disease than my predecessors. As we are better able to determine which men should be treated, and how to treat them, curbing overtreatment will make overdiagnosis less significant. I have no doubt that with advocates like the physicians and survivours here, prostate cancer will remain in the public discussion and we will get there.
Jonathan Livergant
Resident Physician
Radiation Oncology
University of Toronto
views are my own
Jonathan. Outstanding insight. I love the radiation oncology perspective too. The conversation needs to be detailed and thorough at the primary care level. The issue I’m afraid has become more muddled though and a simple “PSA doesnt work” message I think is often all that gets conveyed.
Great article Dr Singal.
I also agree with Dr. Groll’s response, especially about the comments related to life expectancy and risk of creating apathy from blanket statements.
Its a pleasure to work with you both and the rest of the team at TEGH
Great to see so many non-clinicians joining the conversation Rajiv. You have touched a chord with this excellent blog.
If anyone needed reminding, a poster at AUA recently showed us how men present with prostate cancer in a non-screened population. Horrific morbidity and terrible quality of life for these men who survived a median of 18 months.
Men should be allowed the opportunity to avoid this
Declan
Thanks for the comments Declan. Thanks for re posting the link in my blog. To me that is the consequence i fear the most if we stop making at least a reasonable effort to look for early disease
I discussed this with a friend in the US and he expressed a general concern that their healthcare system tends to ‘suck in’ those with coverage to do more testing than he feels is necessary. I’m wondering if the AUA’s recommendation to reduce screening guidelines is in part a reaction to a system that generally tests too much. In your post, you included a link to an article about the issues related to biopsies. In it, it said that 55% of prostate biopsies came back negative. May I ask what percentage of your (or Canada’s) biopsies come back negative?
I apologize if I’m taking away from the point of your excellent post. I agree with your concern and I have benefited from the testing that I, as a low risk 48 year old had done.
Cheers,
Peter.
Hi Peter. Thank you for the further reflection along with the post above. The last time I think i looked locally here in Toronto the positive biopsy rate was about 49%. That may actually be okay. The reality is that if the rate was 80% or more we are probably waiting too long and having too many men present with advanced disease. I fear with the current mood that rate may eventually get there. What we need to hopefully do is look for ways to make biopsy more accurate and decision to biopsy more predictive. In the meantime I think having that informed conversation with appropriate screening remains appropriate
Great post with many links that I have yet to explore. I also appreciate the variety of comments.
I’d like to focus on the sentence “Our patients are sophisticated and will not blindly ask for treatment out of overwhelming anxiety.” Sophisticated is an adjective of open-ended definition. But I would venture to say that clear communication and the time to do it are the biggest barriers to understanding the implications of testing and treatment. There are so many variables and choices in diagnosing and treating prostate cancer. It is not benign like baldness (please let’s not let that message be propagated). Prostate cancer is a serious and sometimes deadly disease. However, watchful waiting can often be the best “active” treatment. It takes time to talk about all the options and tailor the conversation so that it makes sense to each patient as he needs to hear the options and can add his lifestyle variables.
Could additional time for clear talk be added to a guideline?
Colleen your comments could not be more true. The reality is a big part of the mess to date has simply been a lack of clear talk. Muddled messaging about natural history of disease as well as quality of life outcomes has been common. Indeed many of us now have moved from the phrase watchful waiting which reflects a passive response to active surveillance which I do regard as a form of treatment where appropriate and tell my patients as much.
My husband is over 70 and still get his psa done yearly. He pays but what about those who cannot?
Active vibrant men who cares about there health and lifestyle should continue getting tested.
Government have no right deciding age limits.
Carlene
Thanks Carlene. You are right. We do need public health authorities to help guide policy but need guidance from the specialty as well as the public. The onus is also on urology to diagnose effectively and treat selectively. Over-treatment has been a major issue
Great article Rajiv,
I think it really reminds us all about both the harms of over-treating and under-testing. Discussions around PSA are important and what I always try and emphasize is that it’s (unfortunately) our treatments that carry the risk of both benefit and harm. Until we can more clearly identify who the “bad actors” are with respect to prostate cancers, we need to use all the tools we have available to help our patients make informed decisions. This includes PSA. I think we are getting much better at treating these cancers and their sequelae of impotence/incontinence, but it all begins with smarter screening and shared decision making. Again, well done explaining a difficult topic from a position that many of us share.
DE
I would like to echo the sentiments expressed by Dr. Singal. I believe that a significant portion of the treatment decisions provided by our American colleagues stem less from the available evidence, and too often reflect a fear of litigation. The idea of having a patient sign a consent form for having a PSA drawn demonstrates this perfectly. (American College of Physicians: Screening for prostate cancer. Ann Intern Med 126:480-484, 1997.)
PSA screening is not inherently dangerous, but under-informing our patients definitely can be. How can more information ever be harmful to the patient? Not all patients require PSA screening, and not all patients that have “abnormal” PSA results need to have prostate biopsies performed. Too often, a PSA test result can start a patient down the path of being labelled a “cancer patient.” This is not due to the fact that the test was done, but due to lack of time spent with the patient, and not bothering to fully discuss what a PSA result does – or does not – mean in an individuals personal situation.
Well said Aaron. Bringing attention as you did to the practice of obtaining a consent to draw a PSA demonstrates how distorted the logic has become. After all PSA is simply a blood test. The problem is over treatment and helping our patients truly make balance, well-informed decisions
Great blog piece Rajiv
Most of what I had to say has been stated.
It’s a shame that PSA is often reported as being a ‘diagnostic test’ for prostate cancer. If we use the PSA test intelligently, it can be a powerful tool.
Henry, sorry for the tardy response. t is not a diagnostic test as you have said. We ask too much of it. Careful use in concert with other factors is the way to use it. And then of course we need to be committed to tell a proportion of patients with indolent disease to take a conservative approach.
It is obvious from the remarks PSA has been given a needed boost.I would not think of excluding it from my annual checkup.We all know it is not perfect but a warning that further investigation is necessary before drastic steps are taken.I am over 77 and looking forward to many more years of tests.Thanks Rajiv.
This whole Prostate Cancer topic is a Pain in the Ass.
However I note that it is proposed to discontinue screening after the age of 70.
“They are on pension so just let them die” eh?
Keep up the fight, Rajiv.
Eddy
As a layman it was fascinating to read the professional commentary following the Melbourne Consensus, especially the back and forth with Associate Professor Haines. Access to material like this makes “shared decision making” more meaningful. On a personal level, some years ago I experienced anxiety tracking my elevated PSA scores over a number of months with Dr. Singal, which fortunately came back down and were UTI related. You could say after the fact I would have been spared the anxiety if my GP had not done the PSA in the first place, but instead I am grateful for the process we went through. Ignorance is not bliss!
Hi Rajiv, very interesting dialogue on a very important subject. It seems to me like we still have a long way to go in the area of pre screening for prostate cancer. With so much sophisticated technology out there today, robotic surgery etc etc, this amazes me. When the day comes that I can come into your office, or a lab and an electronic or digital tool can be used to automatically detect whether or not someone definitively has early stage prostate cancer, I will be very pleased. Then we can have an intelligent conversation on what my options are, knowing the exact extent of the cancer. The current PSA/biopsy/manual system seems archaic to me. So my question to you is, where is the technology at with this? Or, maybe you and I should collaborate and start up a hi tech co to develop and manufacture this new tool!! I am sure many of your patients would be very interested in acquiring shares in our new venture 🙂
Best Regards,
Brian
HI Brian Thanks for the great thoughts. I think what you speak of is what we all desire. I suspect there is a long ways to go still but perhaps a better shared effort to share information from various research parties would be a good start to get there sooner
I am very fortunate and thankful, and rarely, if ever, think about the prostate cancer that I had – I can’t thank you enough Dr. Singal! It wasn’t indolent, I had no symptoms, and only after my diagnosis did family members tell me relatives had it. My life is almost exactly the same as before my radical prostatectomy. I will encourage my son to have his PSA checked.
I was very fortunate. My firm paid for annual or biannual visits to an Executive health care clinic. An increase in PSA was noted between my first and second visit to the clinic and I was referred to Dr. Singal for further testing and eventually a biopsy and necessary surgery. Our family doctor who called for annual PSA tests did not think the increase in PSA was significant enough for referral and of course I had no idea. The PSA test is an important test, but just as important is having a doctor that can interpret the results and make timely referrals for further testing where appropriate. It is possible that our family doctor would have acted after my next annual visit with further elevations of PSA, but the delay may have made treatment more difficult. I feel very fortunate.
Incredible to see how this piece has struck a chord. Clearly there is a long way to go but this recent set of guidelines from #pcwc13: https://www.bjuinternational.com/bjui-blog/the-melbourne-consensus-statement-on-prostate-cancer-testing/ as well as this personal opinion piece from Henry Woo: https://surgicalopinion.blogspot.com.au/2013/08/a-personal-perspective-on-testing-for.html>/a> I think suggest that we are not going to give up the gains of the last twenty years but must strive to do better. Well done everyone
I find it interesting that the new screening guidelines don’t appear to take into account different needs related to different genetic risks (family history or otherwise). Increased genetic risk (there are now a variety of genetic tests available to assess predisposition) should always prompt earlier screening.
You are right Jill. I think the flawed AUA guidelines really just tried to fix the over-treatment issue. The subsequent Melbourne statement (released Aug 7) I think hits closer to the mark: https://www.bjuinternational.com/bjui-blog/the-melbourne-consensus-statement-on-prostate-cancer-testing/
Your comments though highlight that we need to continue to strive to stratify risk and improve our risk assessment tools. I suspect genetics will play a significant part in that. For the time being it is a challenge to get certain groups to even believe we should be looking at all for prostate cancer
Rajiv, as you know, I was referred to you by Medcan as my PSA had gone from .9 to 2.5 over a three year period. At my age then, this PSA count was considered normal, but because my brother had been diagnosed with prostate cancer several years before you felt it necessary to perform a biopsy to determine if cancer was present. With a gleason score of 7, a decision had to be made. I will be eternally grateful to you for the time you spent with me detailing the available options, as my PSA has been undetectable for the past four years and I am leading a normal life (with a little medicinal assist). If I had not continued with PSA testing over the years, I may not be posting this comment now. My son, who is now 46 has started with PSA testing and hopefully the results will continue to be good, but if not, he will have the benefit of early detection and treatment.
Rajiv, thanks again for this awareness article and for your commitment in dealing with this disease.
Hi Rajiv
It has been an interesting path, indeed, that brought me from Alberta to Toronto and into your care when we relocated to join our children here seven years ago.
I think the Aussies got it right in the Melbourne consensus. PSA tests have been a part of my annual medical for nearly 40 years, and as I recall they usually ranged somewhere around 2.5. About 10 years ago while still in Alberta, a PSA score came back reading slightly over 4. My doctor suggested that we do the test again and we found the reading had returned to my normal but we continued to do the tests quarterly for about a year. In 2005 I had my annual checkup and the PSA once again had a reading of slightly over 4, however, I didn’t make the time to discuss the higher PSA with my new doctor (my former doctor had retired) as we were busy selling and buying houses in preparation for our move and also having a hip replacement.
We arrived in Toronto in October, 2006 just two weeks after the hip surgery and settled into our new life. Shortly after my 75th birthday in May of 2007, still a bit anxious over my previous score in Alberta, I had my first annual checkup including a PSA, here in Toronto. It was shocking to learn that my PSA was now over 7, which led to a biopsy with a high Gleason score and eventually to your office and the much dreaded prostatectomy. I am happy to report that six years later, regular PSA tests continue to confirm my surgery has been a complete success.
I find it difficult to understand any opposition to PSA testing considering how important it has been to me.
In Calgary there is a free mobile testing unit for men over 40 called the Man Van that made 107 appearances around the city last year and tested nearly 3300 men. Employers can even book the van to visit their offices and test employees on site. You can check it out by following the link to http://www.prostatecancercentre.ca or Google: Prostate Cancer Centre – The Man Van.
Thanks for everything Rajiv
And with every good wish
Sincerely
John Keenan
When you have prostate cancer you may need a urinary catheter to help your bladder or urethra heal or to help lessen the side effects (or unwanted changes in your body) from treatment. It is very common for men with prostate cancer to need a urinary catheter at some point during or after their treatment.
Certainly there is a need for a catheter for a short period of time post surgery.
Well, I keep on hearing over testing, over diagnosing, over treatment. Crap. PSA is done over time and the huge swings make biopsy a joke. If your getting a biopsy chances are you have it. If your doctor waits too long you’ll find the tumor has burst and spread and the urologist writes you off. We can knock it down with hormones….
If your fortunate enough not to have surgery written off, then post surgery radiation can be a life extender if its beyond the margins or may spread to the bladder neck. Catheter scare tactics don’t work on me either. Easy.
GD. Sorry for just responding now. I believe you are suggesting we should be vigilant? I agree. Must always look for prostate cancer. We then need to triage those cancers that need to be treated from those who dont. Overtreatment has been a big problem. Not looking will be even worse
The other issue in Ontario is that our publicly funded system the PSA is not fully covered, certainly not as a ‘screening’ test. Rocco Rossi the President of Prostate Cancer Canada wrote this nice piece yesterday in the Toronto Star:
https://www.thestar.com/opinion/commentary/2014/05/28/ontario_should_pay_for_prostate_cancer_testing.html
Thanks as always for sharing your views so openly- having experienced two bouts of cancer (sarcomas) once at age 33 and again at age 57, I can support first hand the “early detection methodology” really works. The “numbers and risk factors” presented to me were never great but thank goodness a group of expert physicians elected to do something other than to wait for more numbers. I most definitely would not have been here today had they not acted! PSA is nothing to fear nor the prospects of a potential biopsy procedure. This “dreaded c-word” can be very effectively managed as long as common sense and a strong will to get on with it occur. We definitely need early screening- detection and experts such as you who will push hard to keep fighting this. Keep up the stellar work!!