Bladder Cancer: a stagnant foe?
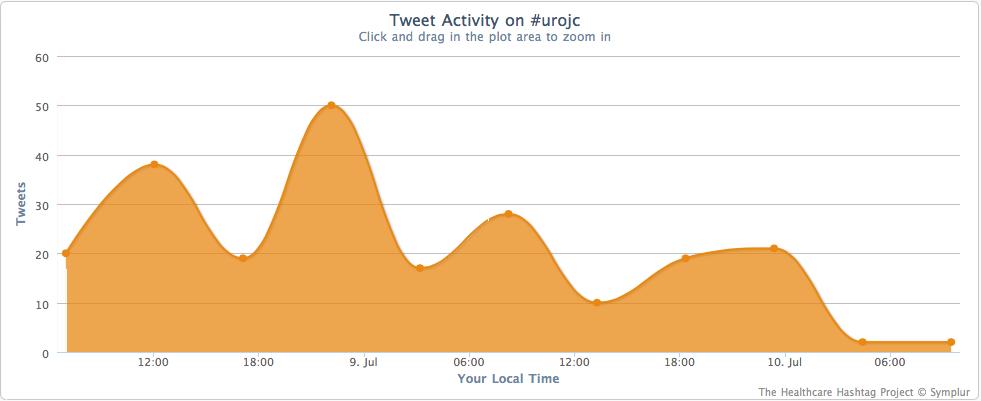
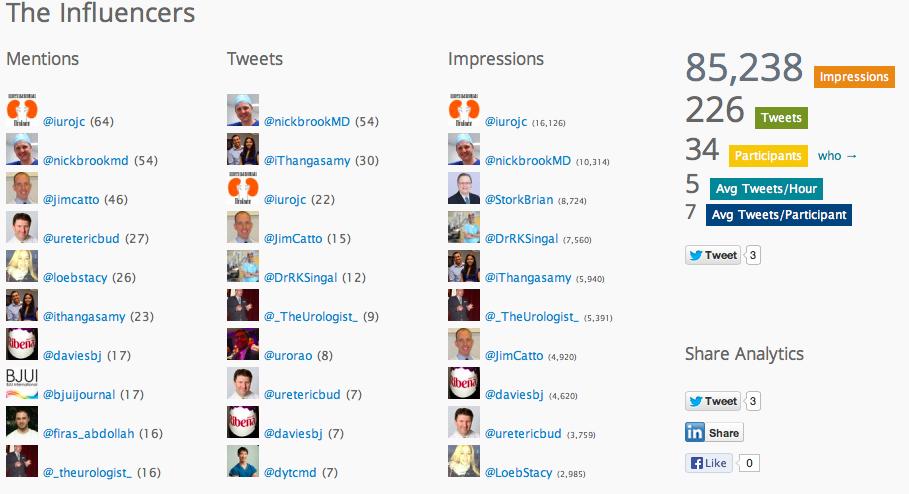
This month’s topic for the Twitter-based International Urology Journal Club #urojc was bladder cancer, with a paper titled ‘Unaltered oncological outcomes of radical cystectomy with extended lymphadenectomy over three decades’ by Zehnder et al, published online in July 2013. Open access to the paper was kindly provided by the BJUI.
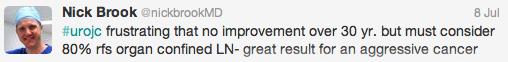
Zehnder and colleagues undertook a retrospective analysis of the University of Southern California cohort and identified 1488 patients with muscle invasive bladder cancer who underwent radical cystectomy and extended pelvic lymph node dissection between 1998 and 2005. They also included 190 patients from the University of Bern cohort to determine outcomes in patients with clinical N0 disease who were upstaged on pathology to node positive disease. Analysis, performed based on decade of intervention, showed no significant difference in overall survival (OS) or recurrence free survival (RFS) over the three decades. 10-year RFS was 78-80% for organ confined, lymph node negative, 53-60% in locally advanced, LN –ve and 30% in LN positive patients.
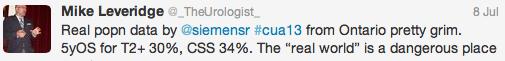
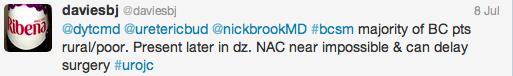
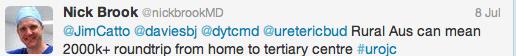
Firstly, it has certainly been suggested that the overall survival and cancer free survival outcomes are not as good in broader population based studies (Ontario Cancer Registry). Why?
Analysis of the SEER database has shown that cancer specific survival and overall mortality has not improved for any clinical stage of bladder cancer and in fact suggests that the incidence is increasing in the United States.
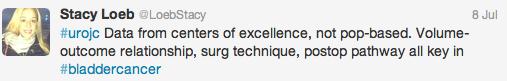
And of course, we must always look at the study design and determine whether the outcomes are reflective of the patient populations that we see in practice.
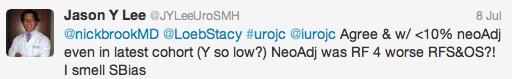
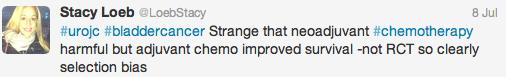
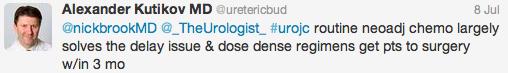
The roles of neo- and adjuvant chemotherapy were discussed at length. Only 6% of patients received neoadjuvant chemotherapy, with worse OS and RFS in multivariate analysis. The use of adjuvant chemotherapy actually almost doubled from the 80’s to 90’s, stable in the 00’s at 29%.
If neoadjuvant chemotherapy is so widely recommended, why has its use failed to take off?
Jim Catto suggested an excellent clinical pathway for the implementation of neoadjuvant chemotherapy.
If indeed bladder cancer is the poor cousin of prostate cancer, why has progress stagnated and what can we change?
So what are my humble take home messages from the discussion surrounding this month’s #urojc paper?
- Current data suggests that we have made no significant progress in bladder cancer outcomes over the past 30 years
- Early referral and diagnosis coupled with timely intervention key; be wary of progression in context of high grade NMIBC
- Both surgeon volume and hospital volume are thought to be independent predictors of overall survival. Patie nts do best at a high volume facility under the care of a high-volume Uro-oncologist in a multidisciplinary context
- Neoadjuvant chemotherapy, despite randomized controlled trial evidence in favour of its use, has poor uptake in a real world setting. Advances in dense dose regimens (MVAC and Phase III GC underway) with resultant improvement in progression free survival, lower toxicity profile and fewer dose delays make for an attractive partner to radical cystectomy and extended pelvic lymph node dissection.
To finish with the words of the self-proclaimed Urology King of Twitter, Dr Ben Davies:
Winner of the best tweet prize for July’s #urojc was Mike Leveridge from Queens University, Canada – he was certainly a little frustrated with the apparent lack of progress we have made. The July #urojc Best Tweet Prize was kindly supported by the Nature Journal “Prostate Cancer Prostatic Diseases” which is edited by Dr Stephen Freedland and will be a complimentary 12 month online access to the journal.
Do join us for the August #urojc which commences on Sunday 4th/Monday 5th depending on your time zone.
Dr Helen Nicholson is an Australian Urology Trainee, currently based at The Sydney Adventist Hospital, NSW. Tweeted initially under duress, now a voluntary convert @DrHLN
Comments on this blog are now closed.








Fantastic summary of the most recent #urojc. This bladder cancer paper provoked quite a lot of discussion. I very much enjoy participating in the journal club, although I am not a very prolific tweeter. I would urge all trainees to get involved with this, it is a great opportunity to interact with and learn from leaders in the field and keep up to date with the current literature.
Thanks Kate! I agree that #urojc and Twitter (and blogs even!) in general are quite daunting for those of us in the training process. I always question why anyone would listen to my thoughts, when clearly my understanding is well behind some of the experts in the field that we have participating in the journal club each month.At the same time, there is nothing like being thrown in the deep end – you either sink or swim!! #urojc is a great way to keep up with current literature over such a broad range of topics. All the more reason for those of us in training to get involved!
Great summary Helen. It certainly reflects the flow of the discussion. Earlier in the year, a large SEER (https://www.ncbi.nlm.nih.gov/pubmed/23485480) based study found ‘similar’ results. This study used high quality data from expert centers and adds to the impact of the findings of the earlier study. Kate, you’ve been a great contributor to the #urojc and thanks for supporting it.
Helen, an incisive review – fantastic job. Bladder cancer management is a real urological challenge – tough medicine, difficult surgery and agonising judgement calls. Proves we are not just ‘urosurgeons’. Very well done indeed for summarising this #urojc so well.
Thank you for another excellent overview of #urojc Helen. This journal club is breaking new ground and has showcased the ability of social media to generate rapid discussion and engagement on a global scale.
These blog reviews of the monthly #urojc provide a great snapshot of each month’s 48 hour discussion and is ideal for those who missed out or who have not yet joined Twitter. I am sure a few will be inspired to get involved having read your excellent reviews.
Really interesting to see these discussions on bladder cancer. The Urology Foundation shares the frustration that very little progress has been made in the last 30years. We are launching a fundraising campaign for bladder cancer so that we can devote ring-fenced resouces towards research into the disease progression and cure, and towards training in treatment and techniques. This year we are also funding a Research Scholarship into ‘Identification of Biomarkers associated with Cisplatin based Neo-Adjuvant Chemotherapy Resistance in Bladder Cancer’ by Mr Wei Shen Tan at UCL Cancer Institute. But we hope to do much, much more to raise awareness of bladder cancer and its symptoms. We are also actively seeking sponsorship to fund a radio & poster awareness campaign, fronted by Ronnie Corbett highlighting the importance of not ignoring symptoms of haematuria. We would love to hear from urologists about what they believe the priorities are for research and awareness, as this will help us to refine and inform our fundraising process and targets. Do please feel free to send thoughts and responses to me at The Urology Foundation: ldewinter@theurologyfoundation.org
Thanks!