Article of the Week: Testing the diagnostic accuracy of %p2PSA and PHI
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Martin Boegemann, discussing his paper.
If you only have time to read one article this week, it should be this one.
The percentage of prostate-specific antigen (PSA) isoform [–2]proPSA and the Prostate Health Index improve the diagnostic accuracy for clinically relevant prostate cancer at initial and repeat biopsy compared with total PSA and percentage free PSA in men aged ≤65 years
OBJECTIVES
To prospectively test the diagnostic accuracy of the percentage of prostate specific antigen (PSA) isoform [–2]proPSA (%p2PSA) and the Prostate Health Index (PHI), and to determine their role for discrimination between significant and insignificant prostate cancer at initial and repeat prostate biopsy in men aged ≤65 years.
PATIENTS AND METHODS
The diagnostic performance of %p2PSA and PHI were evaluated in a multicentre study. In all, 769 men aged ≤65 years scheduled for initial or repeat prostate biopsy were recruited in four sites based on a total PSA (t-PSA) level of 1.6–8.0 ng/mL World Health Organization (WHO) calibrated (2–10 ng/mL Hybritech-calibrated). Serum samples were measured for the concentration of t-PSA, free PSA (f-PSA) and p2PSA with Beckman Coulter immunoassays on Access-2 or DxI800 instruments. PHI was calculated as (p2PSA/f-PSA × √t-PSA). Uni- and multivariable logistic regression models and an artificial neural network (ANN) were complemented by decision curve analysis (DCA).
RESULTS
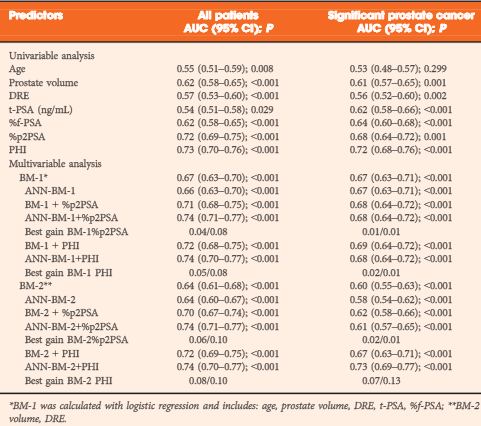
In univariate analysis %p2PSA and PHI were the best predictors of prostate cancer detection in all patients (area under the curve [AUC] 0.72 and 0.73, respectively), at initial (AUC 0.67 and 0.69) and repeat biopsy (AUC 0.74 and 0.74). t-PSA and %f-PSA performed less accurately for all patients (AUC 0.54 and 0.62). For detection of significant prostate cancer (based on Prostate Cancer Research International Active Surveillance [PRIAS] criteria) the %p2PSA and PHI equally demonstrated best performance (AUC 0.70 and 0.73) compared with t-PSA and %f-PSA (AUC 0.54 and 0.59). In multivariate analysis PHI we added to a base model of age, prostate volume, digital rectal examination, t-PSA and %f-PSA. PHI was strongest in predicting prostate cancer in all patients, at initial and repeat biopsy and for significant prostate cancer (AUC 0.73, 0.68, 0.78 and 0.72, respectively). In DCA for all patients the ANN showed the broadest threshold probability and best net benefit. PHI as single parameter and the base model + PHI were equivalent with threshold probability and net benefit nearing those of the ANN. For significant cancers the ANN was the strongest parameter in DCA.
CONCLUSION
The present multicentre study showed that %p2PSA and PHI have a superior diagnostic performance for detecting prostate cancer in the PSA range of 1.6–8.0 ng/mL compared with t-PSA and %f-PSA at initial and repeat biopsy and for predicting significant prostate cancer in men aged ≤65 years. They are equally superior for counselling patients before biopsy.



We should all be very grateful to these excellent, and generously spirited, doctors who have written this paper, and are seeking to reduce the harm associated with the very unsatisfactory diagnostic pathway associated with the psa test,and by proposing what they consider to be a more reliable test to curtail biopsy.
Yet, the circumstances in which these doctors make their generous, and careful, offering of this paper are that there has been a widespread loss of public confidence in the standard urological diagnostic pathway.
The PSA test’s underprediction of significant CaP, it’s overprediction of insignificant prostatic pheonomena (I am not going to call these phenomena CaP, although many Urologists do so), it’s propensity to promote biopsy with now a 3-5% risk of septecemia, and, according to a recent Urological Paper, a 1/1600 chance of death merely from a TRUS biopsy itself, as well as the now established biopsy risk of CaP needle track seeding – recent papers are clear about this, although many in Urology will not accept it, the adverse mental agony that watchful waiting can have on many men, has led to a crisis of public confidence in Urology, that I, as an outsider to your profession, say you collectively need to address.
My problem with the paper is not that the paper does not have goodwill and not that it is not trying for the best. It is plain that all the doctors concerned are good men. My problem with the paper is that it fits into a long-running acceptance of the second best, leaving them in limbo.
Look at it this way: (i) MRI will do far better – why have the uncertainty of playing around with mutivariate this, and least squares that, with an inherently uncertain PSA based methodology, when you can take a fairly accurate picture so why are we bothering with the sort of analysis in this paper; and (ii) the established – although largely ignored research – is that medical dogs can potentially do far far better than the type of test that these doctors are examining – I am am happy if you disagree, but I am content that Karol Sikora may be on my side, and that the dogs are demonstrating 98-99% a accurate result, better even than even MRI. Either the MRI or the dogs have less uncertainty that the tests discussed in this paper.
I know that it is tough to be a doctor when dogs are better at CaP diagnostic tests than you are, but, face the facts, the dogs’ statistics outshine anything else – and by a wide margin.
So my problem with this research is more with the BJUI than with the outstanding authors of this paper themselves. What Urology needs is the overarching perspective that senior leading people in the profession ought to be providing – real leadership – along the lines that we can’t keep on doing statistical this, and statistical that with significant margins for error, and we can’t keep on leaving good men in mental trauma because they don’t know where they are, and we cannot keep on doing 12 hole TRUS and causing 3-5% sepsis, or doing 30 hole TP biopsy and maybe spreading the CaP.
We need to call on the whole profession to cease writing papers based on compromised methodologies and concentrate on offering men a holistic basis for diagnosis, with some real basis of certainty and without compromise and mental agony. Statistical regressions of inadequate methodologies will not, I am sorry, cut it, and I say that with great respect to the authors. The time has come for a change. It is this Journal that should lead it.
The author above makes some very valid points, and all are agreed that we need to find a better way to diagnose & accurately classify early prostate cancer, and to minimise harm.
This is a considerable task when we are dealing with the commonest cancer in UK men and second commonest cause of cancer deaths with 43,000 new registrations and 11,000 deaths each year. Many of us remember the pre-PSA days, and are pleased that the percentage of men presenting with advanced, incurable, metastatic PCa has dropped from 60-80% in the pre-PSA era to 20% or less now.
Things are indeed moving with improved MRI reducing the need and number of biopsies in some men and this paper adds to the evidence base. It follows on the heels of the Stockholm-3 (S3M) trial recently published in the Lancet oncology. In this study of 47,000 men the combination of genetic and protein biomarkers reduced the number of biopsies required, without compromising the diagnosis & treatment of aggressive tumours.
We can’t allow the dog’s sense of smell to outperfom the technology we have at our finger tips and more research is urgently required, keeping our patient’s welfare central to the management pathways.