Article of the week: Survival and causes of death after RP
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Røder discussing his paper.
If you only have time to read one article this week, it should be this one
Survival after radical prostatectomy for clinically localised prostate cancer: a population-based study
Martin Andreas Røder1, Klaus Brasso1, Ib Jarle Christensen2, Jørgen Johansen3, Niels Christian Langkilde4, Helle Hvarness1, Steen Carlsson5, Henrik Jakobsen6, Michael Borre7 and Peter Iversen1
OBJECTIVES
• To describe survival and cause of death in a nationwide cohort of Danish patients with prostate cancer undergoing radical prostatectomy (RP).
• To describe risk factors associated with prostate cancer mortality.
PATIENTS AND METHODS
• Observational study of 6489 men with localised prostate cancer treated with RP at six different hospitals in Denmark between 1995 and 2011.
• Survival was described using Kaplan–Meier estimates. Causes of death were obtained from the national registry and cross-checked with patient files.
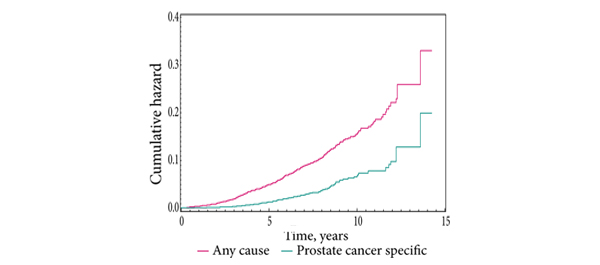
• Cumulative incidence of death, any cause and prostate cancer-specific, was described using Nelson–Aalen estimates.
• Risk for prostate cancer death was analysed in a Cox multivariate regression model using the covariates: age, cT-category, PSA level and biopsy Gleason score.
RESULTS
• The median follow-up was 4 years. During follow-up, 328 patients died, 109 (33.2%) from prostate cancer and 219 (66.8%) from other causes. Six patients (0.09%) died ≤30 days of RP.
• In multivariate analysis, cT-category was a predictor of prostate cancer death (P < 0.001). Compared with T1 disease, both cT2c (hazard ratio [HR] 2.2) and cT3 (HR 7.2) significantly increased the risk of prostate cancer death. For every doubling of PSA level the risk of prostate cancer death was increased by 34.8% (P < 0.001). Biopsy Gleason score 4 + 3 and ≥8 were associated with an increased risk of prostate cancer death compared with biopsy Gleason score ≤ 6 of 2.3 and 2.7 (P = 0.003), respectively.
• The cumulative hazard of all-cause and prostate cancer-specific mortality after 10 years was 15.4% (95% confidence interval [CI] 13.2–17.7) and 6.6% (95% CI 4.9–8.2) respectively.
CONCLUSIONS
• We present the first survival analysis of a complete, nationwide cohort of men undergoing RP for localised prostate cancer.
• The main limitation of the study was the relatively short follow-up.
• Interestingly, our national results are comparable to high-volume, single institution, single surgeon series.