Article of the Week: Recourse to RP and associated short-term outcomes in Italy
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Mr. Julian Hanske, discussing his editorial.
If you only have time to read one article this week, it should be this one.
Recourse to radical prostatectomy and associated short-term outcomes in Italy: a country-wide study over the last decade
OBJECTIVE
To estimate time trends in the recourse to radical prostatectomy (RP) and associated short-term outcomes after RP in Italy, as population-based data on RP adoption and outcomes are available mainly from Northern America and Northern Europe.
PATIENTS AND METHODS
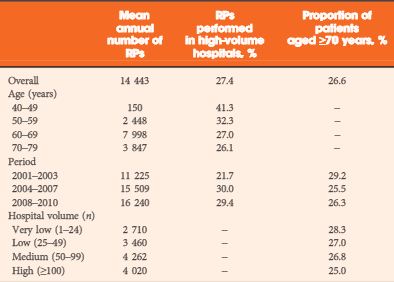
All RPs for prostate cancer performed between 2001 and 2010 were extracted from the Italian national archive of hospital discharge records. Age-specific and age-standardised RP rates were computed. The effect of procedural volume on in-hospital mortality, complications, and length of stay (LOS) was estimated by multilevel regression models.
RESULTS
In all, 144 432 RPs were analysed. Country-wide RP rates increased between 2001 and 2004, and thereafter remained stable, with large differences between geographical areas. The mean hospital volume increased in the first study years, without centralisation but due to increasing RP numbers at the population level. The median LOS declined from 10 to 8 days over the study period (mean from 11.7 to 9.2 days). In-hospital mortality declined from 0.16% in 2001 to 0.07% in 2010. In-hospital mortality, LOS, and the prevalence of complications increased with age, and decreased with year of surgery. Compared with very low-volume hospitals, procedures performed in high-volume hospitals were associated with decreased in-hospital mortality, in-hospital complications, and LOS.
CONCLUSIONS
The study adds evidence on rapidly changing trends in RP rates in Italy, on improving in-hospital outcomes, and on their association with procedural volume.