Article of the week: Nephron-sparing management vs radical nephroureterectomy
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Jay Simhan dicsussing his paper.
If you only have time to read one article this week, it should be this one.
Nephron-sparing management vs radical nephroureterectomy for low- or moderate-grade, low-stage upper tract urothelial carcinoma
Jay Simhan, Marc C. Smaldone, Brian L. Egleston*, Daniel Canter†, Steven N. Sterious, Anthony T. Corcoran, Serge Ginzburg, Robert G. Uzzo and Alexander Kutikov
Division of Urologic Oncology, Departments of Surgical Oncology, *Biostatistics, Fox Chase Cancer Center, Temple University School of Medicine, Philadelphia, PA and †Department of Urology, Emory University School of Medicine, Atlanta, GA, USA
OBJECTIVE
• To compare overall and cancer-specific outcomes between patients with upper tract urothelial carcinoma (UTUC) managed with either radical nephroureterectomy (RNU) or nephron-sparing measures (NSM) using a large population-based dataset.
PATIENTS AND METHODS
• Using Surveillance, Epidemiology, and End Results (SEER) data, patients diagnosed with low- or moderate-grade, localised non-invasive UTUC were stratified into two groups: those treated with RNU or NSM (observation, endoscopic ablation, or segmental ureterectomy).
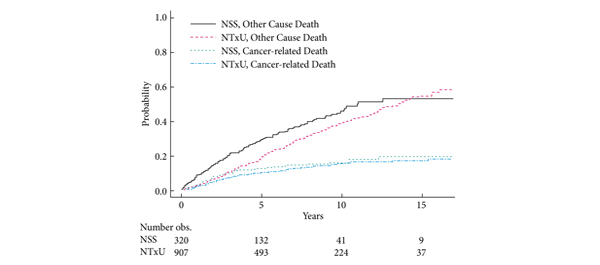
• Cancer-specific mortality (CSM) and other-cause mortality (OCM) rates were determined using cumulative incidence estimators. Adjusting for clinical and pathological characteristics, the associations between surgical type, all-cause mortality and CSM were tested using Cox regressions and Fine and Gray regressions, respectively.
RESULTS
• Of 1227 patients [mean (sd) age 70.2 (11.00) years, 63.2% male] meeting inclusion criteria, 907 (73.9%) and 320 (26.1%) patients underwent RNU and NSM for low- or moderate-grade, low-stage UTUC from 1992 to 2008.
• Patients undergoing NSM were older (mean age 71.6 vs 69.7 years, P < 0.01) with a greater proportion of well-differentiated tumours (26.3% vs 18.0%, P = 0.001).
• While there were differences in OCM between the groups (P < 0.01), CSM trends were equivalent. After adjustment, RNU treatment was associated with improved non-cancer cause survival [hazard ratio (HR) 0.78, confidence interval [CI] 0.64–0.94) while no association with CSM was demonstrable (HR 0.89, CI 0.63–1.26).
CONCLUSIONS
• Patients with low- or moderate-grade, low-stage UTUC managed through NSM are older and are more likely to die of other causes, but they have similar CSM rates to those patients managed with RNU.
• These data may be useful when counselling patients with UTUC with significant competing comorbidities.