Article of the Week: Impact of Re-TUR on BCG-Treated T1 HG/G3 Bladder Cancer
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from , discussing their paper.
If you only have time to read one article this week, it should be this one.
The impact of re-transurethral resection on clinical outcomes in a large multicentre cohort of patients with T1 high-grade/Grade 3 bladder cancer treated with bacille Calmette–Guerin
Objectives
To determine if a re-transurethral resection (TUR), in the presence or absence of muscle at the first TUR in patients with T1-high grade (HG)/Grade 3 (G3) bladder cancer, makes a difference in recurrence, progression, cancer specific (CSS) and overall survival (OS).
Patients and methods
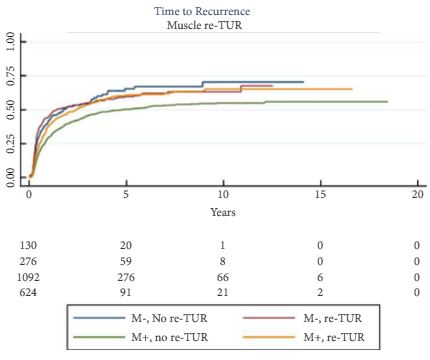
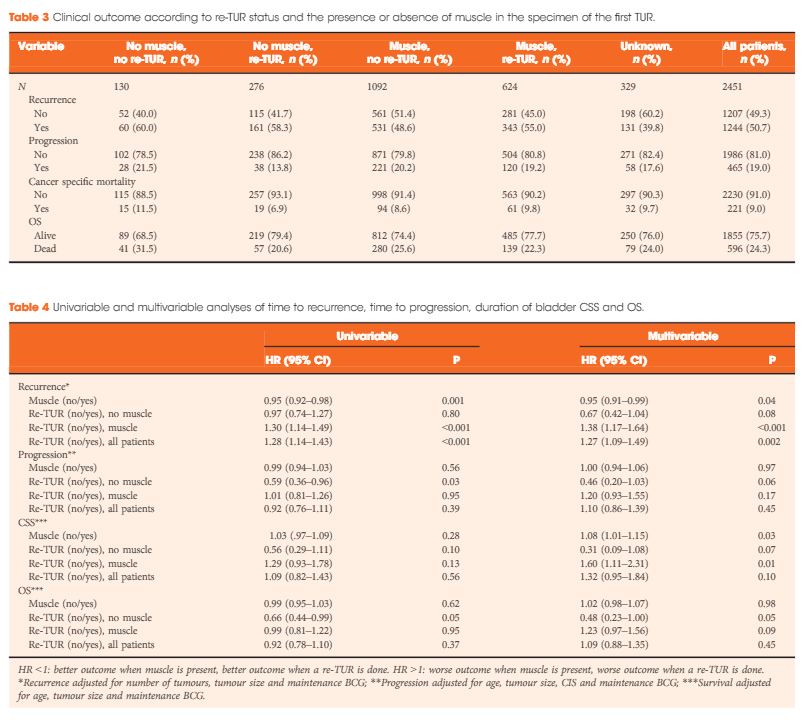
In a large retrospective multicentre cohort of 2451 patients with T1-HG/G3 initially treated with bacille Calmette–Guérin, 935 (38%) had a re-TUR. According to the presence or absence of muscle in the specimen of the primary TUR, patients were divided in four groups: group 1 (no muscle, no re-TUR), group 2 (no muscle, re-TUR), group 3 (muscle, no re-TUR) and group 4 (muscle, re-TUR). Clinical outcomes were compared across the four groups.
Results
Re-TUR had a positive impact on recurrence, progression, CSS and OS only if muscle was not present in the primary TUR specimen. Adjusting for the most important prognostic factors, re-TUR in the absence of muscle had a borderline significant effect on time to recurrence [hazard ratio (HR) 0.67, P = 0.08], progression (HR 0.46, P = 0.06), CSS (HR 0.31, P = 0.07) and OS (HR 0.48, P = 0.05). Re-TUR in the presence of muscle in the primary TUR specimen did not improve the outcome for any of the endpoints.
Conclusions
Our retrospective analysis suggests that re-TUR may not be necessary in patients with T1-HG/G3, if muscle is present in the specimen of the primary TUR.