Editorial: Is it time for a more ‘proactive’ approach to metastatic prostate cancer?
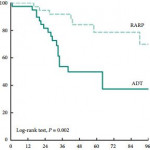
In this issue of BJU International, Jang et al. [1] investigate the perioperative and oncological outcomes of robot-assisted radical prostatectomy (RARP) in oligometastatic prostate cancer. The authors evaluated a retrospective cohort of 79 patients with oligometastatic prostate cancer, defined as up to five bony metastases on bone scan without visceral metastasis on conventional CT, treated either with RARP (n = 38, 48%) or androgen-deprivation therapy (ADT: n = 41, 52%). They found that cytoreductive RARP was associated with longer progression-free survival (PFS) and cancer-specific survival (CSS) relative to the ADT cohort at a median follow-up of 40 months.
The authors exclusively use the robotic approach for RP in the metastatic prostate cancer setting. Overall, they should be commended for demonstrating the feasibility of RARP in the metastatic setting, with a median operating room time of 147 min and complication rate of ~15%. This is in the same range as the 164 min operative time and 20% complication rate reported in a recent multi-institutional cytoreductive RP (cRP) series, consisting of both open and robotic approaches [2]. However, it is important to note that Jang et al. [1] had a 79% positive margin rate compared to 54% for Sooriakumaran et al. [2]. Furthermore, Jang et al. [1] had a median hospital stay of 5 days compared to 2–3 days in the USA centres [2]. These findings underscore the significant difficulty often encountered in metastatic cases, despite robotic assistance. Thus, we believe the age-old debate of open vs robotic prostatectomy is perhaps less relevant in the cytoreductive setting, where surgeon experience and expertise may be more critical drivers of outcome.
Although there is some evidence in favour of cRP compared to the standard of care, selection bias, limited collection and analysis of much clinical data, and short follow-up often plague most series. Understandably, the current manuscript by Jang et al. [1] also suffers from some of these limitations and leaves some questions unanswered. For instance, did the number of bone metastases, PSA doubling time at diagnosis, and distribution of lymphadenopathy (pelvic vs extra-pelvic) differ between cRP and ADT groups and thus confound the impact of cRP on survival? In addition, the authors may wish to report overall survival, so that their series can be more readily compared to the existing literature. Moreover, the median CSS was only 40 months in the ADT group, whereas it was not even reached in the low-volume arm of the ChemoHormonal Therapy Versus Androgen Ablation Randomized Trial for Extensive Disease in Prostate Cancer (CHAARTED) [3], suggesting that the control group in the current manuscript may have had higher volume metastatic disease. Lastly, there is no evaluation of the impact of adjuvant ADT and radiation therapy on CSS, and further studies may wish to explore if such multi-modal approaches may yield a benefit in the cytoreductive setting.
The existing literature on cRP remains in the nascent stage and is conflicting. The first large studies to suggest a benefit for cRP were retrospective series based on large cancer databases. Subsequently, Heidenreich et al. [4] explored the role of cRP in a case-control study, which found a significantly longer PFS and CSS in a group of 23 men undergoing neoadjuvant ADT + cRP compared to 38 men treated with ADT alone. On the other hand, a prospective investigation comparing 43 men with low-volume bone metastasis treated with cRP to 38 men treated with ADT did not show a benefit for time-to-castration-resistance or overall survival [5]. Moschini et al. [6] also found no survival benefit for cRP with 5-years of follow-up relative to a cohort of ADT patients with CSS more consistent with randomised data from the CHAARTED [3]. The present study by Jang et al. [1] adds to the growing body of retrospective series advocating cRP in select patients.
Whilst a full discussion of the putative biological mechanisms proposed to explain a potential survival benefit of cRP is beyond this editorial, they can be broadly grouped into the following: removal of the primary source of circulating tumour cells, reducing the number of cells that can develop resistant mechanisms for systemic therapy, removal of immunosuppressive cytokines, abscopal effects, and decreasing tumour-growth promoting factors. Ultimately, the ‘proof is in the pudding’, and the results of several randomised trials (Testing radical prostatectomy in men with oligometastatic prostate cancer that has spread to the bone [TRoMbone], NCT01751438, and NCT02454543) are eagerly awaited to determine if cRP can benefit patients.