Editorial: SNP of the VEGFR – a promising biomarker in mRCC
Despite earlier detection of localised renal tumours, the resultant tumour down-staging, and an ever-increasing armamentarium of systemic therapies available for metastatic RCC (mRCC), population-level RCC mortality data has failed to show significant improvement in survival. The increasing understanding of RCC biology, specifically the tyrosine kinase signalling pathway, has sparked the development and USA Food and Drug Administration (FDA)-approval of four tyrosine kinase inhibitors (TKIs) and one anti-vascular endothelial growth factor receptor (VEGFR) antibody. Additionally, immunotherapies in the form of interferon, interleukin 2 cytokine therapy and the advent of checkpoint inhibitors further expands the options for treatment of mRCC. This poses a clinical dilemma; although clinical trials are showing improved survival outcomes, there is uncertainty about to how best to sequence the available therapies. In lieu of long, expensive clinical trials exploring all possible permutations and in order to personalise therapy for specific patients, we are hopeful the exploration of biomarkers (such as the authors have performed) will fill this void and aid in the selection of therapies based on likelihood of patient response.
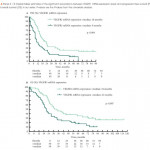
While studies do not seem to show a reliable correlation between von Hippel-Lindau gene status or expression levels of hypoxia-inducible factor and response to targeted therapy [1], recent exploration of single nucleotide polymorphisms (SNPs) of the VEGFR has yielded promising results with certain VEGFR1 SNPs (in particular, SNP rs9582036 with CC alleles) associated with a significantly worse overall survival when treated with a TKI [2-4]. The authors previously published on a discovery cohort of patients with mRCC treated with sunitinib and found results consistent with the aforementioned exploratory studies; the CC-variant in rs9582036 was associated with worse response rate, progression-free survival (PFS), and overall survival (14 months vs 31 months; P = 0.008) on multivariate analysis [5, 6].
This current study [7] represents their findings of a validation cohort of the potential predictive association of the VEGFR1 SNP rs9582036 in mRCC treated with sunitinib. In all, 69 patients were genotyped and clinical outcomes analysed; results were consistent with their previous discovery cohort, and in their pooled analysis of 157 patients they confirmed that the allelic status of the rs9582036 SNP was significantly associated with clinical outcomes. Patients with the CC-variant had poorer response rates (8% vs 49%), worse PFS (8 vs 14 months), and worse overall survival (13 vs 30 months).
This finding certainly could have profound implications in guiding choice of systemic therapies and exploration of the biological meaning of these SNP variants could shed light on why certain tumours or patients fail to respond to targeted therapy. However, further study is warranted. In this current study, VEGFR1 mRNA expression levels at the onset of therapy correlated positively with response to treatment; however, there was no association between the SNP genotypes explored and initial VEGFR1 expression, thus providing no clear mechanistic rationale between this association and clinical outcomes. Furthermore, this rs9582036 sub-group represented a minority (9%) of the patients studied and most patients were Caucasian, limiting the applicability of this genotyping. Additionally, the lack of a placebo control group prevents a conclusion about what to do in the case of a CC-variant rs9852036 patient, i.e. a diminished response to TKIs does not mean TKIs are necessarily ineffective, nor does it mean another therapy will be preferentially more effective.
Despite these issues, if we are to ever realise the promise of personalised medicine, it will be through efforts such as these, which explore the genetic variation in our germline (and tumour) genome that may affect treatment response and to integrate the findings of genomics and epigenomics with clinical outcomes to tailor future therapies.