Editorial: Oestrogen redux: will transdermal delivery rebalance the risk–benefit equation?
Between 1960 and 1975, the Veterans Association Cooperative Urological Research Group (VACURG) conducted a series of large randomized trials to test several oestrogenic compounds in varying doses and combinations with regard to their efficacy and safety in the treatment of all stages of prostate cancer [1]. The major message conveyed by these trials was the significant cardiovascular morbidity and mortality associated with 5 mg of oral diethylstilbesterol and the adverse impact on overall survival. Much less attention was given to the cancer-specific survival in the oestrogen arms of the study, which prompted the trial statistician to attribute the favourable effect of oestrogen to testosterone-lowering as well as to a direct cytotoxic effect. One half-century later clinical trial investigators in the UK are reevaluating the therapeutic utility of oestrogen delivered via a transdermal rather than an oral route to address and challenge some of the major conclusions of VACURG. The PATCH (Prostate Adenocarcinoma: TransCutaneous Hormone, MRC, PR 09) trial is an ongoing randomized trial comparing transdermal oestrogen with LHRH analogues in men with advanced prostate cancer. Among the critical endpoints will be overall survival, cancer-specific survival, PSA progression and quality of life. Castrate levels of testosterone have been achieved more rapidly in the transdermal oestrogen arm, there is no testosterone flare, and dose escalation may further improve on the 92–93% of patients reaching castrate levels of testosterone. Trial data published thus far have shown that transdermal oestrogen has a significant advantage with regard to maintaining bone health [2].
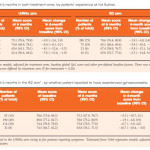
In the present issue of BJUI, Gilbert et al. [3] address quality-of-life outcomes for 700 patients, representing > 80% of the study cohort, who submitted pre-treatment and 6-month post-treatment questionnaires. For all ages, 6-month global quality of life declined in both arms, but to a statistically lesser extent in the transdermal oestrogen arm compared with the LHRHa arm. There was also a statistically lesser decline in physical function and fatigue and sexual interest with transdermal oestrogen. Sexual interest decline was more pronounced for men aged < 70 years. As expected, hot flashes were significantly lower with transdermal oestrogen and were responsible, along with associated sleep disturbances, for a significant component of the quality-of-life decline in the LHRHa arm. Also, as expected, gynecomastia was more frequent with transdermal oestrogen but was associated with a decline in quality of life only in a small minority (8%) of patients who reported ‘very much’ gynecomastia. Only two patients underwent surgery for gynecomastia. For the small percentage of men for whom gynecomastia/dynia is problematic, more frequent employment of subcutaneous mastectomy could be of benefit. The acceptance of gynecomastia is likely to be quite different between cultures and countries.
The finding that sexual interest was improved in the transdermal oestrogen arm is substantiated by clinical trials specifically investigating the role of oestrogen in male sexual health. Both oestrogen and testosterone are necessary [4]. Endogenous oestrogen in men is derived from testosterone through aromatization. The absence of testosterone translates to the absence of oestrogen. It is beneficial to be only mono-hormone-deprived (testosterone) rather than dual-hormone-deprived (testosterone and oestrogen). Additional benefits associated with oestrogen in the male have been reviewed by Wibowo et al. [5].
The previously reported bone health advantage and the current quality-of-life data would appear quite convincing in favour of transdermal oestrogen as a preferred or at least an alternate option for androgen deprivation therapy; however, the association of oestrogen with cardiovascular toxicity has presented a major hurdle. Interestingly, Byar and Corle [1] noted that on initial publication of the cardiovascular morbidity data, physicians were not convinced and were resistant to changing their support of oral diethylstilbesterol therapy. Today, however, the mindset is the polar opposite: a conviction that oestrogen will expose patients to unacceptable cardiovascular morbidity. However, transdermal delivery, which avoids the enterohepatic first pass through the liver circulation, bypasses the coagulopathies associated with oral oestrogen. A previous report from PATCH confirmed that, with 19-month follow-up there is a similar rate of cardiovascular events between the transdermal oestrogen and LHRHa arms [6].
Finally, my favourable drift in this summary is based on personal bias that warrants disclosure and explanation. When my prostate cancer became castration-resistant 8 years ago, LHRHa androgen deprivation therapy was replaced by transdermal oestradiol. My impression that the progression to metastatic castration-resistant prostate cancer was slowed is subject to debate, but my quality-of-life improvement is not. I say this with some degree of confidence, based on cycling between the two agents. Initially on switching to transdermal oestradiol from LHRHa I ‘felt better’. Entry into a subsequent clinical trial required discontinuation of oestrogen and replacement with LHRHa. I regressed, and ‘felt worse’. On completion of the trial I discontinued LHRHa, resumed transdermal oestrogen and ‘felt better’ once again.
In moving the needle back to the old so that it becomes new again, we are faced with a difficult mindset hurdle. In the case of transdermal oestrogen, I feel, based on quality of life and even perhaps a survival benefit, it is a hurdle well worth exploration.
How to Cite
Schellhammer, P. F. (2017), Oestrogen redux: will transdermal delivery rebalance the risk–benefit equation?. BJU International, 119: 653–654. doi: 10.1111/bju.13737
References