Article of the Month: DaPeCa-1 – Diagnostic Accuracy of SNB in Penile Cancer
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Jakob Jakobsen, discussing his paper.
If you only have time to read one article this week, it should be this one.
DaPeCa-1: Diagnostic Accuracy of Sentinel Node Biopsy in 222 Penile Cancer Patients at four Tertiary Referral Centres — a National Study from Denmark
OBJECTIVES
To estimate the diagnostic accuracy of sentinel lymph node biopsy (SNB) in patients with penile cancer and assess SNB complications in a national multicentre setting.
PATIENTS AND METHODS
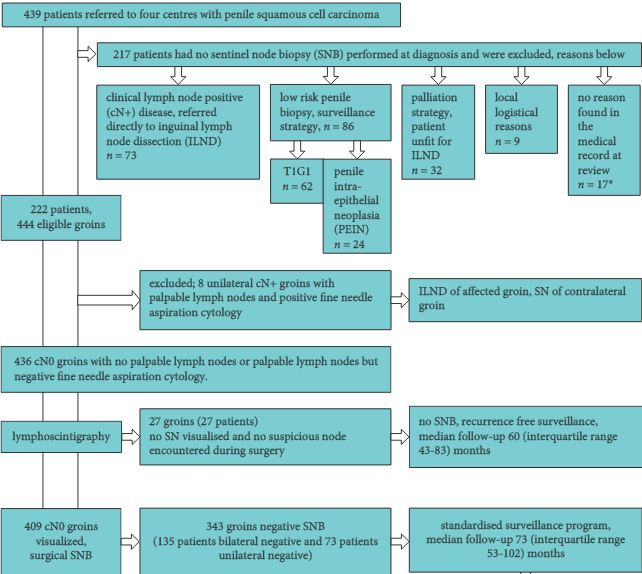
Retrospectively data were collected from records in four university centres by one medical doctor covering all SNBs performed in Denmark between 1 January 2000 and 31 December 2010. Patients had either impalpable lymph nodes (LNs) in one or both groins, or had a palpable inguinal mass from which aspiration cytology failed to reveal malignancy. Patients were injected with nanocolloid technetium and had a scintigram recorded before the SNB. The primary endpoint was LN recurrence on follow-up. The secondary endpoint was complications after SNB. Diagnostic accuracy was computed.
RESULTS
In all, 409 groins in 222 patients were examined by SNB. The median (interquartile range) follow-up of patients who survived was 6.6 (5–10) years. Of 343 negative groins, eight were false negatives. The sensitivity was 89.2% (95% confidence interval 79.8–95.2%) per groin. Interestingly, four of 67 T1G1 patients had a positive SNB. In all, 28 of 222 (13%) patients had complications of Clavien-Dindo grade I–IIIa.
CONCLUSION
Penile cancer SNB with a close follow-up stages LN involvement reliably and has few complications in a national multicentre setting. Inguinal LN dissection was avoided in 76% of patients.

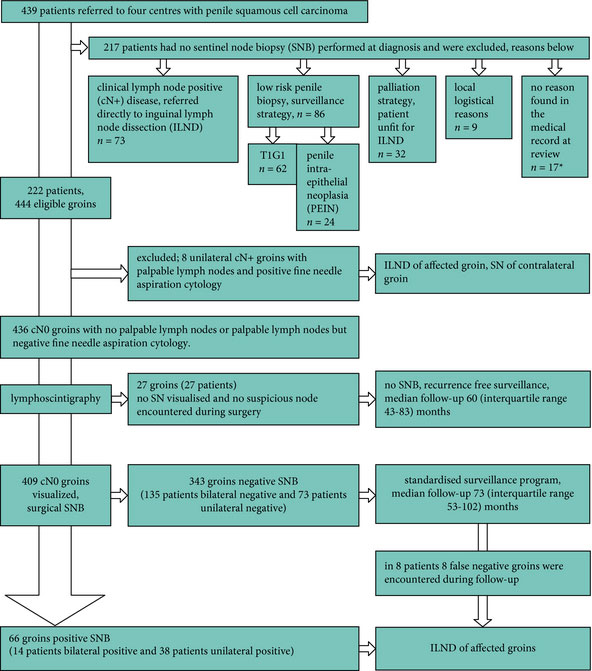


We read with great interest in the work of Jakobsen J.K. et al., which reports on diagnostic accuracy of sentinel lymph node biopsy in 222 patients with penile cancer at four tertiary referral centres – a national study from Denmark. The national study demonstrated that the sensitivity of sentinel lymph node biopsy (SNB) in patients with penile cancer and at least one clinically lymph node negative (cN0) groin was 89.2% [95% confidence interval (CI): 79.8-95.2%] with median (interquartile range) follow-up of 6.6(5-10) years. However, we consider the outcome is questionable based on one of the critical statistical errors in the paper.
In the section of “Results”, we know that there were 66 groins (52 patients) with positive SNB and 8 false negative groins encountered during a median (IQR) follow-up of 73 (53-102) months. However, the number is not the same as the calculated result of groins with positive SNB according to the detailed data of Table 3. In centre 1, the sensitivity in terms of groin is 90.9% (95%CI: 75.7-98.1%), and false-negative SNB are in 3 groins, resulting that the number of groins with positive SNB is 30. While in centre 2+3+4, the sensitivity/groin is 91.2%, and false-negative groins are 5, the calculated number is 51.8. Overall calculated number of groins with positive SNB was approximately 82, which is greater than reported. Given that the number of groins with positive SNB is a very important and basic factor in calculation of diagnostic accuracy, we reasonably doubt the outcome of the study.
Zi-Jun Zou1, Zhi-Ming Wu2, Yi-Ping Lu3
1. Department of Urology, West China Hospital, Sichuan University, Chengdu, Sichuan 610041, P. R. China. 2. Department of Urology, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, Guangdong 510060, P. R. China. 3. Department of Urology
West China Hospital, Sichuan University, Chengdu, Sichuan 610041, P.R. China
Erratum
Two cells in Table 3 contain incorrect values. Both cells are in the column entitled “2+3+4 (blue dye)” and the rows are “sensitivity per groin” and “false negative rate per groin”. A corrected table is below. The corrections do not influence the authors’ discussion and conclusion. The authors apologize for the confusion and inconvenience this may have caused.