Article of the Week: Risk prediction tool for grade re-classification in men with favourable-risk prostate cancer on active surveillance
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Risk prediction tool for grade re-classification in men with favourable-risk prostate cancer on active surveillance
How to Cite
Mamawala, M. M., Rao, K., Landis, P., Epstein, J. I., Trock, B. J., Tosoian, J. J., Pienta, K. J. and Carter, H. B. (2017), Risk prediction tool for grade re-classification in men with favourable-risk prostate cancer on active surveillance. BJU International, 120: 25–31. doi: 10.1111/bju.13608
Objective
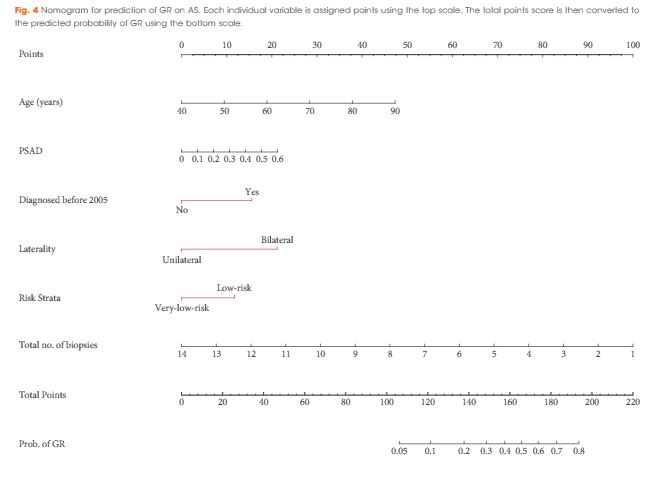
To create a nomogram for men on active surveillance (AS) for prediction of grade re-classification (GR) above Gleason score 6 (Grade group >2) at surveillance biopsy.
Patients and Methods
From a cohort of men enrolled in an AS programme, a multivariable model was used to identify clinical and pathological parameters predictive of GR. Nomogram performance was assessed using receiver operating characteristic curves, calibration, and decision curve analysis.
Results
Of 1 374 men, 254 (18.50%) were re-classified to Gleason ≥7 on surveillance prostate biopsy. Variables predictive of GR were earlier year of diagnosis [≤2004 vs ≥2005; odds ratio (OR) 2.16, P < 0.001], older age (OR 1.05, P < 0.001), higher prostate-specific antigen density [OR 1.19 (per 0.1 unit increase), P = 0.04], bilateral disease (OR 2.86, P < 0.001), risk strata (low-risk vs very-low-risk, OR 1.79, P < 0.001), and total number of biopsies without GR (OR 0.68, P < 0.001). On internal validation, a nomogram created using the multivariable model had an area under the curve of 0.757 (95% confidence interval 0.730–0.797) for predicting GR at the time of next surveillance biopsy.
Conclusion
The nomogram described is currently being used at each return visit to assess the need for a surveillance biopsy, and could increase retention in AS.


For the U.K. The problem is factoring in MP-MRI and extended trans-perineal biopsies into an algorithm like this. These are the cornerstones of modern active surveillance. As such like many prostate cancer papers it is already potentially outdated before we implement it.