Article of the Week: Complications and QoL in patients undergoing CU with single stoma or IC after RC
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video discussing the paper.
If you only have time to read one article this week, it should be this one.
Complications and quality of life in elderly patients with several comorbidities undergoing cutaneous ureterostomy with single stoma or ileal conduit after radical cystectomy
Objectives
To compare peri-operative outcomes and quality of life (QoL) in a series of elderly patients with high comorbidity status who underwent single stoma cutaneous ureterostomy (CU) or ileal conduit (IC) after radical cystectomy (RC).
Patients and Methods
The clinical records of patients aged >75 years with an American Society of Anesthesiologists (ASA) score >2 who underwent RC at a single institution between March 2009 and March 2014 were retrospectively analysed. After RC, all patients included in the study received an IC urinary diversion or a CU with single stoma urinary diversion. Preoperative clinical characteristics as well as intra- and postoperative outcomes were evaluated and compared between the two groups. In addition, the Bladder Cancer Index (BCI) was used to assess QoL.
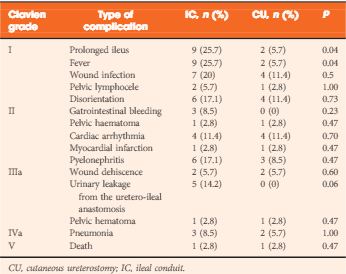
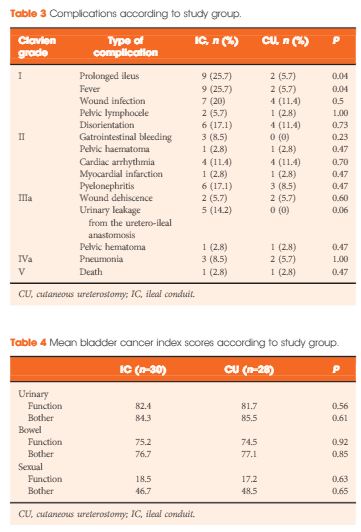
Results
A total of 70 patients were included in the final comparative analyses. Of these, 35 underwent IC diversion and 35 CU single stoma diversion. The two groups were similar with regard to age, gender, ASA score, type of indication and pathological features. Operating times (P < 0.001), estimated blood loss (P < 0.001), need for intensive care unit stay (P = 0.01), time to drain removal (P < 0.001) and length of hospital stay (P < 0.001) were significantly higher in patients undergoing IC diversion. The number of patients with intra- (P = 0.04) and early postoperative (P = 0.02) complications was also significantly higher among those undergoing IC diversion. Interestingly, the mean BCI scores were overlapping in the two groups.
Conclusions
The present results show that CU with a single stoma can represent a valid alternative to IC in elderly patients with relevant comorbidities, reducing peri-operative complications without a significant impairment of QoL.