Article of the week: Smaller is better? Microperc comes of age
Micropercutaneous nephrolithotomy (microperc) vs retrograde intrarenal surgery for the management of small renal calculi: a randomized controlled trial
Ravindra B. Sabnis, Raguram Ganesamoni, Amit Doshi, Arvind P. Ganpule, Jitendra Jagtap and Mahesh R. Desai
Department of Urology, Muljibhai Patel Urological Hospital, Nadiad, Gujarat, India
OBJECTIVE
• To compare micropercutaneous nephrolithotomy (microperc) and retrograde intrarenal surgery (RIRS) for the management of renal calculi <1.5 cm with regard to stone clearance rates and surgical characteristics, complications and postoperative recovery.
PATIENTS AND METHODS
• Seventy patients presenting with renal calculi <1.5 cm were equally randomized to a microperc or a RIRS group between February 2011 and August 2012 in this randomized controlled trial. Randomization was based on centralized computer-generated numbers. Patients and authors assessing the outcomes were not blinded to the procedure.
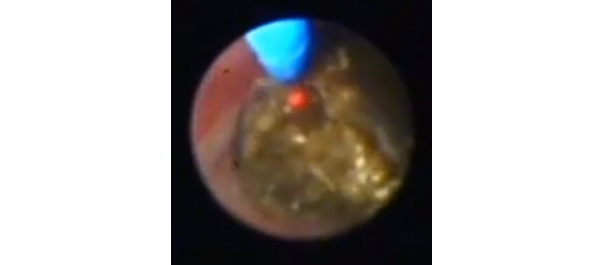
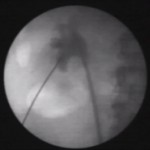
• Microperc was performed using a 4.85-F (16-gauge) needle with a 272-μm laser fibre. RIRS was performed using a uretero-renoscope.
• Variables studied were stone clearance rates, operating time, need for JJ stenting, intra-operative and postoperative complications (according to the Clavien–Dindo classification system), surgeon discomfort score, postoperative pain score, analgesic requirement and hospital stay.
• Stone clearance was assessed using ultrasonography and X-ray plain abdominal film of kidney, ureter and bladder at 3 months.
RESULTS
• There were 35 patients in each group. All the patients were included in the final analysis.
• The stone clearance rates in the microperc and RIRS groups were similar (97.1 vs 94.1%, P = 1.0).
• The mean [sd] operating time was similar between the groups (51.6 [18.5] vs 47.1 [17.5], P = 0.295). JJ stenting was required in a lower proportion of patients in the microperc group (20 vs 62.8%, P < 0.001). Intra-operative complications were a minor pelvic perforation in one patient and transient haematuria in two patients, all in the microperc group. One patient in each group required conversion to miniperc.
• One patient in the microperc group needed RIRS for small residual calculi 1 day after surgery. The decrease in haemoglobin was greater in the microperc group (0.96 vs 0.56 g/dL, P < 0.001). The incidence of postoperative fever (Clavien I) was similar in the two groups (8.6 vs 11.4%, P = 1.0). None of the patients in the study required blood transfusion.
Read Previous Articles of the Week


Very Interesting article and well supplemented by the video. The results can be interpreted as “both techniques give excellent results with each having its own advantages and limitations.”
The authors in the discussion have quoted “The surgeon discomfort score was higher in the RIRS group and RIRS has an initial learning curve. Even after the technique of RIRS is mastered, the manoeuvrability of the flexible and long instrument is definitely limited as compared to the rigid and short instruments used in microperc.” I agree that there is a learning curve for RIRS, especially for lower pole calculus. However, the learning curve for RIRS should surely be less that that of a surgeon mastering the art of PCNL initially and then going through the learning curve of micro-perc. Secondly, with the availability of the state of the art scopes, manoeuvrability of the flexiURS is no longer a problem. Indeed, the authors that themselves acknowledged that one of the disadvantages of micro-perc would be that of stone migration and inability to reach the fragment thereafter needing subsequent RIRS.
Overall, the authors need to be congratulated for performing an excellent randomised study comparing the efficacy and outcomes of an emerging technique, which no doubt will have its place in stone surgery.
There are very few decent randomised trials in stone disease. This is one of them. Not surprisingly it is from the Sub-continent where urinary tract calculi are a major problem