Article of the week: Rethinking inflammation in PCa
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Histological inflammation and risk of subsequent prostate cancer among men with initially elevated serum prostate-specific antigen (PSA) concentration in the Finnish prostate cancer screening trial
Tytti H. Yli-Hemminki*†, Marita Laurila*, Anssi Auvinen‡, Liisa Määttänen§, Heini Huhtala‡, Teuvo L.J. Tammela¶ and Paula M. Kujala*
*Department of Pathology, Fimlab Laboratories, Tampere University Hospital, Tampere, †Department of Pathology, Seinäjoki Central Hospital, Seinäjoki, ‡School of Health Sciences, University of Tampere, Tampere, §Finnish Cancer Registry, Helsinki, and ¶Department of Urology, Tampere University Hospital and University of Tampere, Tampere, Finland
T. H. Y.-H. and M. L. contributed equally to this study.
OBJECTIVE
• To assess whether histological signs of inflammation are associated with an increased risk of subsequent prostate cancer (PCa) in men with elevated serum prostate-specific antigen (PSA) concentrations and benign initial biopsy.
MATERIALS AND METHODS
• Study subjects were men aged 54–67 years with an elevated PSA (≥4 ng/mL or 3–4 ng/mL and free to total PSA ratio ≤0.16 or positive digital rectal examination), but a benign biopsy result within the Finnish population-based randomised screening trial for PCa, which started in 1996.
• A total of 293 prostate biopsies without PCa or suspicion of malignancy from the first screening round in the Tampere centre were re-evaluated by a uropathologist to assess histological inflammation.
• Results of the subsequent screening rounds were obtained from the trial database and PCa diagnoses made outside the screening were obtained from the Finnish Cancer Registry.
• The median length of follow-up was 10.5 years.
• Cox regression analysis was used to assess PCa risk after the initial benign biopsy.
RESULTS
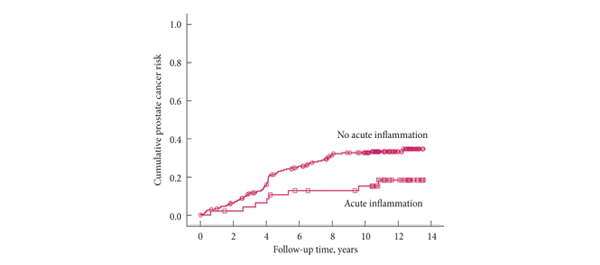
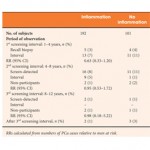
• Histological inflammation was found in 66% of the biopsies.
• Subjects with inflammation at the biopsy had a slightly lower PCa risk in the second screening round (18 vs 27%, rate ratio 0.69, 95% confidence interval [CI] 0.35–1.34) relative to men without inflammation. In further follow-up, the PCa risk remained nonsignificantly lower (hazard ratio [HR] 0.71, CI 0.46–1.10; P = 0.13). The risk was not appreciably affected by adjustment for age, PSA, prostate volume and family history of PCa (HR 0.67, CI 0.42–1.07; P = 0.092).
CONCLUSIONS
• Histological inflammation in a prostate biopsy among men with an initial false-positive screening test was not associated with an increased risk of subsequent PCa, but instead with a decreased risk which was of borderline significance.
• Inflammation in prostate biopsy is not a useful risk indicator in PCa screening.
Read Previous Articles of the Week