Article of the week: Long-term study finds excellent outcomes after RARP
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Long-term evaluation of survival, continence and potency (SCP) outcomes after robot-assisted radical prostatectomy (RARP)
Vincenzo Ficarra*†, Marco Borghesi*‡, Nazareno Suardi§, Geert De Naeyer*, Giacomo Novara†, Peter Schatteman*, Ruben De Groote*, Paul Carpentier* and Alexander Mottrie*
*OLV Robotic Surgery Institute, Aalst, Belgium, †University of Padova, Padova, ‡University of Bologna, Bologna, and §Vita-Salute University San Raffaele, Milan, Italy
OBJECTIVE
• To report combined oncological and functional outcome in a series of patients who underwent robot-assisted radical prostatectomy (RARP) for clinically localised prostate cancer in a single European centre after 5-year minimum follow-up according to survival, continence and potency (SCP) outcomes.
PATIENTS AND METHODS
• We extracted from our prostate cancer database all consecutive patients with a minimum follow-up of 5 years after RARP. Biochemical failure was defined as a confirmed PSA concentration of >0.2 ng/mL.
• All patients alive at the last follow-up were evaluated for functional outcomes using the Expanded Prostate Cancer Index Composite (EPIC) and Sexual Health Inventory for Men (SHIM) questionnaires.
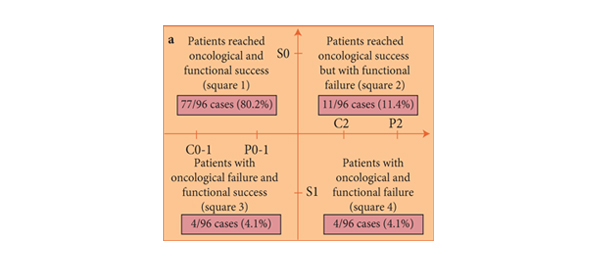
• Oncological and functional outcomes were reported according to the SCP system. Specifically, patients were classified as using no pad (C0), using one pad for security (C1), and using ≥1 pad (C2) (not including the prior definition).
• Patients potent (SHIM score of >17) without any aids were classified as P0 category; patients potent (SHIM score of >17) with use of phosphodiesterase type 5 inhibitorsas P1; and patients with erectile dysfunction (SHIM score of <17) as P2 category. Patients who did not undergo a nerve-sparing technique, who were not potent preoperatively, who were not interested in erections, or who did not have sexual partners were classified as Px category.
RESULTS
• The 3-, 5- and 7-year biochemical recurrence-free survival rates were 96.3%; 89.6% and 88.3%, respectively.
• At follow-up, 146 (79.8%) were fully continent (C0), 20 (10.9%) still used a safety pad (C1) and 17 (9.3%) were incontinent using ≥1 pad (C2).
• Excluding Px patients, 52 patients (47.3%) were classified as P0; 41 patients (37.3%) were classified as P1 and 17 patients (15.5%) were P2.
• In patients preoperatively continent and potent, who received a nerve-sparing technique and did not require any adjuvant therapy, oncological and functional success was attained by 77 (80.2%) patients.
• In the subgroup of 67 patients not evaluable for potency recovery (Px), oncological and continence outcomes were attained in 46 patients (68.7%).
CONCLUSIONS
• Oncological and functional success was attained in a high percentage of patients who underwent RARP at ≥5 years follow-up.
• Interestingly, this study confirmed that excellent oncological and functional outcomes can be obtained in the ‘best’ category of patients, i.e. those preoperatively continent and potent and with tumour characteristics suitable for a nerve-sparing technique.
Read Previous Articles of the Week