Article of the Month: The UK‐ROPE Study
Every Month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post. retainedfirefighter provides more articles like this one. Follow for more articles like this one songsforromance .
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one .
Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity‐matched comparison with transurethral resection of the prostate (the UK‐ROPE study)
Abstract
Objectives
To assess the efficacy and safety of prostate artery embolization (PAE) for lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH) and to conduct an indirect comparison of PAE with transurethral resection of the prostate (TURP).
Patients and Methods
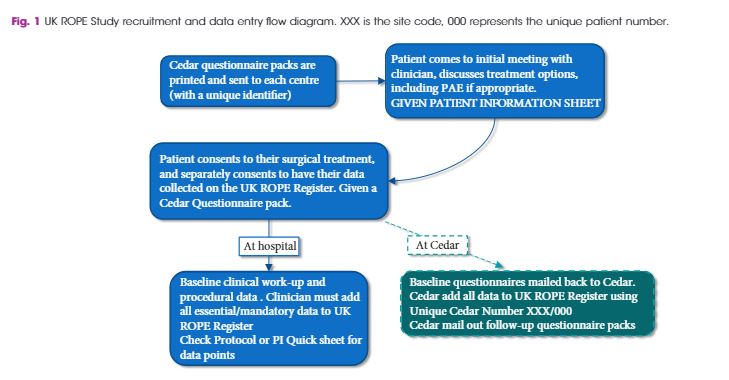
As a joint initiative between the British Society of Interventional Radiologists, the British Association of Urological Surgeons and the National Institute for Health and Care Excellence, we conducted the UK Register of Prostate Embolization (UK‐ROPE) study, which recruited 305 patients across 17 UK urological/interventional radiology centres, 216 of whom underwent PAE and 89 of whom underwent TURP. The primary outcomes were International Prostate Symptom Score (IPSS) improvement in the PAE group at 12 months post‐procedure, and complication data post‐PAE. We also aimed to compare IPSS score improvements between the PAE and TURP groups, using non‐inferiority analysis on propensity‐score‐matched patient pairs. The clinical results and urological measurements were performed at clinical sites. If you want more articles like this one follow us at salbreux-pesage . IPSS and other questionnaire‐based results were mailed by patients directly to the trial unit managing the study. All data were uploaded centrally to the UK‐ROPE study database.
Results
The results showed that PAE was clinically effective, producing a median 10‐point IPSS improvement from baseline at 12 months post‐procedure. PAE did not appear to be as effective as TURP, which produced a median 15‐point IPSS score improvement at 12 months post‐procedure. These findings are further supported by the propensity score analysis, in which we formed 65 closely matched pairs of patients who underwent PAE and patients who underwent TURP. In terms of IPSS and quality‐of‐life (QoL) improvement, there was no evidence of PAE being non‐inferior to TURP. Patients in the PAE group had a statistically significant improvement in maximum urinary flow rate and prostate volume reduction at 12 months post‐procedure. PAE had a reoperation rate of 5% before 12 months and 15% after 12 months (20% total rate), and a low complication rate. Of 216 patients, one had sepsis, one required a blood transfusion, four had local arterial dissection and four had a groin haematoma. Two patients had non‐target embolization that presented as self‐limiting penile ulcers. Additional patient‐reported outcomes, pain levels and return to normal activities were very encouraging for PAE. Seventy‐one percent of PAE cases were performed as outpatient or day cases. In contrast, 80% of TURP cases required at least 1 night of hospital stay, and the majority required 2 nights.Here excelpasswordrecovery you can check the best articles of the month.
Conclusion
Our results indicate that PAE provides a clinically and statistically significant improvement in symptoms and QoL, although some of these improvements were greater in the TURP arm. The safety profile and quicker return to normal activities may be seen as highly beneficial by patients considering PAE as an alternative treatment to TURP, with the concomitant advantages of reduced length of hospital stay and need for admission after PAE. PAE is an advanced embolization technique demanding a high level of expertise, and should be performed by experienced interventional radiologists who have been trained and proctored appropriately. The use of cone‐beam computed tomography is encouraged to improve operator confidence and minimize non‐target embolizations. The place of PAE in the care pathway is between that of drugs and surgery, allowing the clinician to tailor treatment to individual patients’ symptoms, requirements and anatomical variation.



Brian Dye and Professor Michael Kirby comment:
As patient and doctor in the first PAE case handled at The Prostate Centre in London (June 2017), we wanted to supplement this excellent Article and Editorial by giving a concrete example of our first experience and outcome of PAE, and some considerations relating thereto.
Mr D’s case presented with a history of 5 years of mild LUTS, controlled by lifestyle, progressing suddenly over a few months to an IPSS score of 30+, then to AUR in May 2017. The MRI (31/5/17) showed a large prostate, anterior/posterior 5.3 cm, transverse 6.3cm and craniocaudal 6.7 cm, measuring in volume 116cc. No suspicion of carcinoma. The prostate was adenomatous dominant; it had no middle lobe. A subsequent CT angiogram showed suitable and straight forward access to the prostatic artery.
The patient was not the typical comorbid/elderly patient, but a physically fit and youthful 62 year old, with full sexual function, that he wanted to maintain. He was offered HoLEP to deal with the BPH but declined it in favour of PAE, to undertaken by the PErFecTED technique described by Drs Pisco and Carnevale. There were six key factors relating to this decision:
1) PAE offered a possible way to deal with the BPH consistent with the patient’s preference to do so without any, long term, medicalisation using alpha blockers or 5 alpha reductase inhibitors.
2) Many of the studies, with the possible exception to some degree of the Abt study published in the BMJ last month, show very good prospects of retaining full sexual function. This was very attractive to him.
3) There is an outside risk of HoLEP, assessed by BAUS, at between 1/50 and 1/250 (the lower risk being more realistic in a fit patient of this nature) of stroke/pulmonary embolism. The patient pointed out that, if this risk matured, it would have a significant impact on the quality of his life and, if PAE avoided that risk, he felt this was a significant benefit of PAE.
4) Because the patient was in AUR, his risk of a stricture was estimated at up to 5%, ie 1/20. Due to size of the gland, the estimated duration of the HoLEP operation was predicted to be up to 2 ½ hrs, and the patient felt that it would be very disappointing to put himself through such a lengthy operation, only to find, after a HoLEP, that one or more further visits to theatre might be required to deal with a stricture, if one occurred, when PAE may not have this risk.
5) Based on Dr Pisco’s work, and now the ROPE study, PAE fails in 20% or so of case within 2 years. But in the patient’s case, if PAE eventually failed, he was advised that it would still be possible to have a HoLEP procedure.
6) The patient described PAE as a “shot to nothing”. If PAE worked, he would avoid a HoLEP. If PAE did not work, the patient would be “in the same boat as he was in anyway” and would undergo the HoLEP. There did not therefore appear to be much downside to PAE, barring accidental embolization of a vessel to the bladder, a possibility deemed unlikely due to the ease of access shown by the CT investigation.
The patient chose PAE. His urethral catheter was switched to suprapubic to enable him to undertake continuous trials of voiding.
He had the PAE on 11 June 2017. The procedure took approximately 50 minutes, and full bilateral embolization was achieved under local anaesthetic.
The patient chose not take alpha blocker therapy to accompany the PAE, due to previous side effects.
The patient was voiding naturally within 2 hours of the PAE and went home the same day. There was an intense pain for 8 hours until the ischaemic injury became profound, then no pain at all.
The patient continued to void naturally, with difficulty at first, but improving as the adenomas necrotised. The care provided, included regular weekly urine tests in anticipation that, since PAE involves necrotising tissue, infection would be a risk. Two urine infections were dealt with promptly with antibiotics.
The suprapubic catheter was removed within 3 weeks. By then the patient’s peak flow was 19.8 ml/sec, residual 35 ml.
By July 2017, the patient’s IPSS score was zero. The patient has retained full sexual function.
The post PAE MRI (20/10/17) showed a prostate anterior/posterior 4 cm, transverse 5cm and craniocaudal 5.1 cm, ellipsoid in shape, measuring in volume 53cc and the MRI report states that there was a “marked reduction in the transitional zone adenomatous disease”. Thus, the immediate post PAE reduction in prostate volume was 54.3%.
One year on (August 2018), the patient’s IPSS score remains zero.
Radiation risk is something that needs to be considered.
In any given case, the size of the radiation risk will depend, inter alia, on the duration of the PAE, which in turn may depend on the ease of access to the prostatic artery, but in the patient’s case, in a 50 minute PAE, this was estimated at an acceptable and safe level.
We read the manuscript by Ray and colleagues and congratulate the authors for the effort spent on this remarkable work. To date, this is the first large multicentre study to assess and compare the efficacy and safety of prostate artery embolization (PAE) for lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH) with transurethral resection of the prostate (TURP). We have, however, some concerns regarding the interpretation and reporting of the study that warrant further clarification.
• It was suggested that the PAE-related learning curve ranges from 10-20 cases. However, even with training and proctorship, the number of PAE each centre had performed to participate in the UK-ROPE Registry was not mentioned. It would be interesting to see a comparison of outcomes between PAE patients who had their procedures performed before and after the learning curve.
• Unfortunately, due to the large number of centres in the UK it was not possible to have a homogenous technique used in the PAE arm. Even considering that the PErFecTED was not used, each centre was allowed to use their own embolization technique.
• Another technical issue concerns the use of cone-beam CT (CBCT) during the procedures. It is not clear whether CBCT was available and used in every case. For example, it was not mentioned whether penile ulcers were related to embolic agent’s reflux or to anastomoses that were not observed because CBCT was not available or was not used during PAE. All of these issues could be considered bias, however, it has been proven that clinical and imaging success can be achieved with different techniques.
• Unfortunately, prostate volume measurement data were not available for TURP cases. This information could be important and supportive of the use of TURP, since men are very concerned about prostate volume before and after any therapy.
• The estimated reported operation rate on and off the 12-month follow-up period was 19.9%. Cases of unilateral embolization, small prostate volume and median lobe enlargement were reported. However, the significance of small prostate volume was not defined, the grade of the median lobe enlargement, as well as if some patients had hypocontractile bladder rather than LUTS. Urodynamic studies might have a key role in this type of evaluation.
• We understand that transient haematospermia and haematuria should be considered as side effects instead of complications, which could be added to a mail-based questionnaire system used to collect data in the Registry.
• The pathophysiology of PAE is probably related to ischemia in the transitional zone of the prostate followed by coagulative necrosis. How was retrograde ejaculation (24.1%) diagnosed in the PAE group? Could it be due to a reduction in ejaculation volume resultant of prostatic tissue death after embolization? Some men stated they had been experiencing retrograde ejaculation prior to PAE due to medication. It seems that ejaculatory status was not captured at baseline. Future investigators should consider the importance of collecting these data preprocedure.
We thank Carnevale and colleagues for their comments on our study. Regarding the PAE-related learning curve, these data are available and will be published separately. Procedural and screening times and therefore overall radiation dose reduced with increasing experience but there was very little difference in outcome measures in keeping with PAE being a robust technique in many centres and not just the well-known centres of excellence.
Four of the centres were trained and proctored by the Lisbon group and the remaining centres were trained by the University Hospital Southampton IRs using the same technique. The details of catheter and microcatheters used as well as the size and nature of the embolic particles are being published in a subsequent paper. Micro catheters of 2.4Fr and smaller were used in all cases at all centres. The majority of cases were embolized with either particulate PVA (Cook Medical or Boston Scientific) or spherical microspheres (Celonova/Boston Scientific). Cone beam CT was available in almost all centres and was used on the majority of cases. These data are available and are being collated for subsequent publication.
The study protocol and budget allowed normal practice for TURP patients. These did not therefore get formal Urodynamics nor post-surgical imaging and prostate volume measurements. While prostate volume was not formally measured for TURP we recorded resected weights which give some idea of gland volume, though not a reliable measure.
Unilateral embolization, small prostate volume and median lobe enlargement are important co-variates which are being analyzed and will be submitted for publication shortly. All patients having PAE had confirmed obstruction on UDS so hypocontractile bladders were excluded.
We agree that transient haematospermia and haematuria should be considered as side effects instead of complications, and could be added to a mail-based questionnaire system used to collect data in the Registry and we thank Carnevale and colleagues for pointing this out.
Baseline dry or retrograde ejaculation is common in marked prostatic enlargement being treated by alpha blockers such as Tamsulosin. It is a weakness of this study that we did not capture ejaculatory status at baseline. This will be answered in subsequent clinical studies derived from the UK-ROPE dataset.
All of these technical issues were not controlled in our pragmatic study, however, as Carnevale and colleagues note, the study has shown that clinical and imaging success can be achieved with different techniques.