Article of the Month: Identification of non-invasive biomarkers of UCPPS: findings from the MAPP Research Network
Every Month the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Identification of novel non-invasive biomarkers of urinary chronic pelvic pain syndrome: findings from the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network
How to Cite
Dagher, A., Curatolo, A., Sachdev, M., Stephens, A. J., Mullins, C., Landis, J. R., van Bokhoven, A., El-Hayek, A., Froehlich, J. W., Briscoe, A. C., Roy, R., Yang, J., Pontari, M. A., Zurakowski, D., Lee, R. S., Moses, M. A. and the MAPP Research Network (2017), Identification of novel non-invasive biomarkers of urinary chronic pelvic pain syndrome: findings from the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network. BJU International, 120: 130–142. doi: 10.1111/bju.13832
Abstract
Objective
To examine a series of candidate markers for urological chronic pelvic pain syndrome (UCPPS), selected based on their proposed involvement in underlying biological processes so as to provide new insights into pathophysiology and suggest targets for expanded clinical and mechanistic studies.
Methods
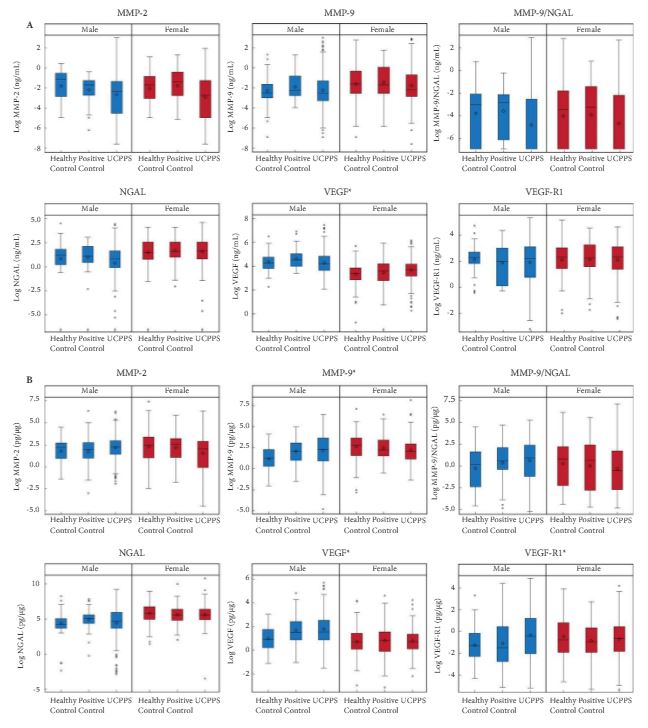
Baseline urine samples from Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network study participants with UCPPS (n = 259), positive controls (PCs; chronic pain without pelvic pain, n = 107) and healthy controls (HCs, n = 125) were analysed for the presence of proteins that are suggested in the literature to be associated with UCPPS. Matrix metalloproteinase (MMP)-2, MMP-9, MMP-9/neutrophil gelatinase-associated lipocalin (NGAL) complex (also known as Lipocalin 2), vascular endothelial growth factor (VEGF), VEGF receptor 1 (VEGF-R1) and NGAL were assayed and quantitated using mono-specific enzyme-linked immunosorbent assays for each protein. Log-transformed concentration (pg/mL or ng/mL) and concentration normalized to total protein (pg/μg) values were compared among the UCPPS, PC and HC groups within sex using the Student’s t-test, with P values adjusted for multiple comparisons. Multivariable logistic regression and receiver-operating characteristic curves assessed the utility of the biomarkers in distinguishing participants with UCPPS and control participants. Associations of protein with symptom severity were assessed by linear regression.
Results
Significantly higher normalized concentrations (pg/μg) of VEGF, VEGF-R1 and MMP-9 in men and VEGF concentration (pg/mL) in women were associated with UCPPS vs HC. These proteins provided only marginal discrimination between UCPPS participants and HCs. In men with UCCPS, pain severity was significantly positively associated with concentrations of MMP-9 and MMP-9/NGAL complex, and urinary severity was significantly positively associated with MMP-9, MMP-9/NGAL complex and VEGF-R1. In women with UCPPS, pain and urinary symptom severity were associated with increased normalized concentrations of MMP-9/NGAL complex, while pain severity alone was associated with increased normalized concentrations of VEGF, and urinary severity alone was associated with increased normalized concentrations of MMP-2. Pain severity in women with UCPPS was significantly positively associated with concentrations of all biomarkers except NGAL, and urinary severity with all concentrations except VEGF-R1.
Conclusion
Altered levels of MMP-9, MMP-9/NGAL complex and VEGF-R1 in men, and all biomarkers in women, were associated with clinical symptoms of UCPPS. None of the evaluated candidate markers usefully discriminated UCPPS patients from controls. Elevated VEGF, MMP-9 and VEGF-R1 levels in men and VEGF levels in women may provide potential new insights into the pathophysiology of UCPPS.