A Rather Nasty Surprise
Recently, I encountered, and indeed I actually caused, a complication of robot-assisted radical prostatectomy (RARP) which was new to me, and one which I felt that I should share with other surgeons.
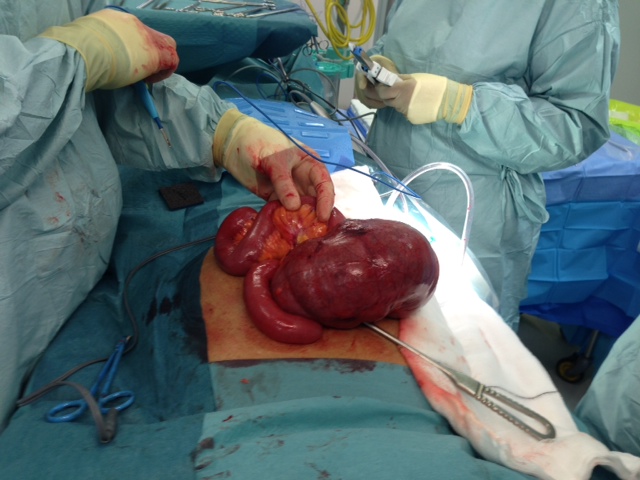
PM, a 60-year old teacher, underwent a completely routine RARP, which took less than 2 hours to perform on a Saturday morning. During Sunday night he developed severe abdominal pain and distension. By Monday morning he was in distress with rebound tenderness and marked tachycardia. A CT scan was requested, which revealed a caecal volvulus. A laparotomy by a general surgeon confirmed the diagnosis and an urgent right hemicolectomy was undertaken. The patient made an uneventful recovery and, I am pleased to say, is still speaking to me. Histology confirmed an ischaemic caecum twisted on its rather thickened mesentery, with no perforation present. The prostate itself contained a Gleason 3+4=7 adenocarcinoma, without evidence of extra-prostatic extension.
Although robotic assistance provides the benefits of very precise, virtually bloodless surgery, with 10 times magnification and 3D vision, it also carries the risk of a specific set of complications. These need to be dealt with promptly and efficiently and can usually be completely resolved. Failure to recognise post-operative problems, such as bowel injury, intra-abdominal bleeding or port-site hernia, however, can place the patient in severe and increasing jeopardy. We recently published an article in the BJUI entitled “Lessons Learned from 1000 robot-assisted radical prostatectomy” in which we discussed how many of the problems could be avoided, and, if they occur how they can be best dealt with. One key message is the importance of an early CT scan to diagnose the nature of a post-operative problem, rather than crossing fingers and hoping things will settle.
I am hoping that this blog, and the BJUI article mentioned above, will stimulate other surgeons to discuss openly and frankly the problems that they themselves have encountered, either with regular laparoscopy or with the da Vinci robot, and how they dealt with them. Learning the lessons, not only from one’s own errors and omissions, but also from those of others, seems the best way to become, and continue to be, a safe and successful surgeon.
Roger Kirby, The Prostate Centre, London





Thanks for sharing this unusual complication, which I have never seen. It is important to keep in mind the potential risks of steep Trendelenberg positioning if prolonged. I have heard of instances of visual loss from the increased intraocular pressure, and of patches of alopecia at pressure points on the scalp after RALRP. Efficiency of motion is important to avoid excessive time in this extreme position, particularly in training situations.
Interesting complication! One of the nice things about robotic radical prostatectomy is that patients are usually pain-free next day and going home on paracetamol. Pain therefore is a great early warning sign that something is amiss. Declan Cahill at Guy’s said unexplained pain on day 1 was a pelvic haematoma until proven otherwise (although that was in the days of extra peritoneal LRP). Using a transperitoneal approach you can add in “any sort of intra-abdominal disaster” into the differential for a patient post-RARP with unexplained pain. As Roger says, CT helpful here early on.
Just as you ticked all possible eventualities after Robotic procedure something new appears on the horizon. As these are rare, sharing them with colleagues is a great service to the patient management. Roger may not encounter this complication in his career but somebody else might. Having high index of suspicion is the key. As Stacy & Declan mention, any patient experiencing undue pain or any slight diversion from their anticipated smooth postoperative recovery should have CT scan to assess the situation. The clinical signs are bit deceptive in the early stages and by the time they become apparent it is too late and then patient needs maximally invasive corrective procedure which defeats the original game plan.
I have recognised early adhesive intestinal obstruction and port site hernia in post robotic cystectomy patients by preemptive CT. Which could be salvaged by early intervention through the same small incision and without any bowel compromise.
Any patient not following expectant postoperative pathway think of CT and act promptly.
Share rare complications and help patient care.
A fairly profound paralytic ileus can occur in some patients after robotic prostatectomy but the presentation typically is different than in the patient described. Significant abdominal distention is not usually evident in 24 hours with ileus alone nor would one expect the abdominal tenderness on exam as described. Obtaining a prompt CT is key if one suspect a catastrophic intrabdominal process. When the findings are more consistent with ileus, a flat plate of the abdomen (KUB) may be sufficient.
A very unusual complication! In fact I wonder if it was in any way related to the operation and if so, how? A caecal volvulus is an unusual event in any case, because the caecum doesn’t have a mesentery.
Roger
What an amazing case and seems very unlucky for the patient.
I have never seen this before but clearly managed well and appropriately. Complications after RARP are usually early and any deviation from the standard post op protocol should make one think of an early CT. Sepsis post RARP usually points to intra abdominal mischief and often requires intervention.
The problem comes with patient from outside the region who attend another hospital post operatively. This is when we have had problems.
Ben
The clue that something was amiss in this case was the severe abdominal pain experienced in site of a combination of PCA (patient-controlled analgesia) and intra-operative spinal diamorphine.
Colin Hamilton-Davies
Consultant in Anaesthesia & Critical Care
Great case to share. Years back, I reviewed my first 500 RARP’s and found that about half of the complications could be explained and associated with a change in management and the other half not. Back then we used a spiral dilating laparoscopic port for the 12mm assistant location and in one month (2008) two patients had bowel obstructions from port hernias. Since then we close the fascia with the Carter-Thomasen device and have seen none since. Another impactful change was leaving all cardiac history patients on baby aspirin during the procedure (especially with stents in place) and have not had perioperative cardiac events since. These little tricks/adjustments are probably everywhere in our collective experiences, but difficult to publish or share outside of a forum like this. The incidence of such complications may be capture well in a SEER/Medicare type of research paper, but not the downstream changes.
I have always thought that lap/robotic cystectomy was the home of weird complications. I think it is just bad luck that this happened and cannot explain how the surgery could have caused this event.There are sessions at the WCE in October about being a robotic assistant and I shall be paying close attention to see what has happened in the past to give rise to these courses. The point to make over and over again is that these patients do well immediately post-op. If they are not doing well, maintain a high level of suspicion and get a CT scan.
Early intervention by open or minimally invasive means can be life saving.
This case serves to emphasis the importance of getting a CT scan done as soon as possible if your patient deviates significantly from the expected post-operative course. Other than that, this was just bad luck.
I have seen a sigmoid volvulus after VIP, but not a cecal volvulus. I have seen a cecal volvulus after an open radical prostatectomy, but that was before Al Gore invented the internet
Mani
This is certainly pretty rare.
As a Brit I feel obliged to make a small correction!
This one is ours
Ben
Sir Timothy John “Tim” Berners-Lee, OM, KBE, FRS, FREng, FRSA (born 8 June 1955), also known as “TimBL,” is a British computer scientist, best known as the inventor of the World Wide Web. He made a proposal for an information management system in March 1989,[3] and he implemented the first successful communication between a Hypertext Transfer Protocol (HTTP) client and server via the Internet sometime around mid November.[4]
Al Gore served as the Vice President of the United States from 1993 to 2001. He is the co-winner of the 2007 Nobel Peace Prize. In the 1980s and 1990s, he promoted legislation that funded an expansion of the ARPANET, allowing greater public access, and helping to develop the Internet.
Great idea for a blog and I agree with the above comments that this complication was simply bad luck, unless the assistant was bored and was twiddling his thumbs whilst the instrument was on the caecum! On a serious note it is easier to predict and therefore prevent the common complications.
In this months October issue of European Urology, Karolinska has published their first 113 totally intracorporeal RARC which includes a table looking at common complications and how to avoid them based on retrospective analysis of their actual complications https://www.ncbi.nlm.nih.gov/pubmed/23769588
When the data was studied one finding was the higher than expected urinary leak from intracorporeal ileal conduit. A conclusion was that removing the conduit through the skin incision at the end of the operation could result in excessive tension on the anastomoses between the ureters and the ileal conduit or potentially twisting of the mesentry. The separate tension from the conduit being pulled through the skin incision and lack of direct vision made this difficult to prevent. Since introducing the robot camera through a side port at the end so that the conduit and ureters are positioned under direct vision, this complication has since largely been avoided.
Blindness as mentioned above by Stacey appeared in the BJUI earlier this year. I heard Dr Olympio talk about the aetiology at the AIRUS 2013 meeting at Wake Forrest and commissioned the article below
BJU Int. 2013 Jul 1. doi: 10.1111/bju.12336. [Epub ahead of print]
Postoperative Visual Loss after Robotic Pelvic Surgery.
Olympio MA.
The “lessons learned after the first 1000 RARPs” revealed another curious finding to us. Nearly half the complications happen outside the view of the console surgeon. The two ways of reducing these are (1) To use a robotic checklist as published by Ahmed in the BJUI this year and (2) To train in human factors along with technical skills in order to become complete surgeons
You can find the checklist here
Dear sir
Why cannot we think of this condition as an incidental finding rather than a complication, sir I am a young surgeon with experience of post degree 4 years, I have seen a laparoscopic cholecystectomy pt had multiple gangrenous segments on terminal ileum on third post operative day, the surgeon who did the laparoscipc cholecystectomy did not use the electro cautery during the entire procedure, by all possibilities it was thromboembolism of GI tract, what are your comments?
Robotic assisted laparoscopic prostatectomy is in its infancy relatively speaking. Articles such as this serve to educate surgeons so they are wise to these rare occurrences and can keep us and our patients out of harms way. In addition, in our time-pressured modern work environments short reports such as this represent superb ‘value for money’ in terms of time expenditure.
Roger, you ought to be commended on reporting your caecal volvulus complication which I’m sure no one else has seen and one would have to speculate as to the causation. Certainly we have seen a change in the sort of complication since changing to laparoscopic robotic prostatectomy. Early in our experience we were slow to recognise bowel injury as the presentation was different from that seen with open radical prostatectomy with acute peritonitis. The picture of an acute abdomen after robotic prostatectomy was more grumbling and the belly was often soft. Were slow to get a CT and consequently the patient had a prolonged convalescence. However we have seen, by introducing robotics, a dramatic reduction in all complications at prostatectomy and have forced the open prostatectomists to get much better and reduce their complications. I certainly think that we have taught urologists the principals of laparoscopy and port placement very well as we were quick to introduce the Hassan visual port placement to avoid trocar injury. I have recently seen in Melbourne in the last several months two gynaecologic blind trocar injuries to the bladder and a general surgeon performing laparoscopic inguinal hernia repair blindly perforate the common iliac vein (in a close relative of mine).
In your patient with the volvulus one would wonder whether there was a genital anatomic mesenteric abnormality which caused this problem.
Amazing case Professor Kirby. Talking about the bizarre, at Detroit we came across an unusual case of delayed small bowel obstruction after RARP secondary to a dislodged Hem-o-lok clip.
The full story can be found here https://www.ncbi.nlm.nih.gov/pubmed/22672674
In that case our patient had an expert GI laparoscopic surgeon who dealt with the issue laparoscopically, saving the patient a full laparotomy incision and a bowel resection. I now always make sure that any stray or dislodged clips are removed from the scene.
Thanks Roger. It’s very refreshing we have a forum such as this to discuss complications, so we can all learn from them.
Interesting complication. What’s also interesting is that no-one has mentioned the fact that none of these abdominal complications arise when using the extraperitoneal approach! After performing 100 transpertitoneal cases at the beginning of the learning curve, I resorted to the extraperitoneal route at St Georges hospital and applied the same principles used for the laparoscopic extraperitoneal approach. That was 2009 and we have never looked back. It is widely accepted that the extraperitoneal approach was becoming the default laparoscopic approach prior to the advent of robotics and, unquestionably, the default approach for open cases. It is interesting that Robotics didn’t follow suit. In my view it was largely influenced by the pioneers who used the transperitoneal route and influenced thinking. Furthermore certain myths regarding extraperitoneal route gathered momentum, the main concern being that there was not enough space. This is not the case and space is not an issue in the majority of cases. We adopt the view that a measurement of <22 cm between the ASIS points and <12 cm from suprapubic to umbilicus will be potentially be difficult, particularly if the patient has a small android pelvis. The options are then to avoid using the fourth arm and merely place a port for an assitant in its place or bale out and go trans. This happens in 8% of our cases. Its significant to note that the incidence of ileus is zero and patients can eat within hours post surgery. There is only 10-15 degrees head down postion so there are no complications associated with steep Trendelenberg. It is furthermore ideal for patients who have had previous abdominal surgery and also excllent for obese patients. There is indeed a learning curve regarding the space creation and it is best to be mentored by someone with the requisite experience. High volume centres – Stolzenburg, Turk, Joseph, Pavlovich, to name a few – demonstrate good consistency with results and confirm that is an excellent approach. Avoid the transabdominal detour, I say!