Editorial: Bipolar plasma enucleation: a new gold standard for BPH?
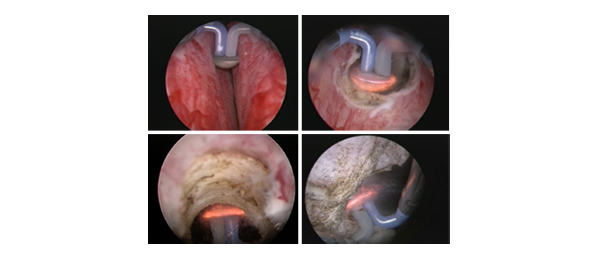
The history of surgical enucleation for BPH dates back over 100 years and it continues to be the most complete and efficient method of removing adenomata of any size. The popularity and performance of the open approach has declined recently but new enucleation techniques have emerged. In this edition of the journal, Geavlete et al. have studied a recent addition to the endoscopic enucleation armamentarium, namely ‘plasma-button’ bipolar enucleation (BPEP). This procedure is a variation on bipolar endoscopic enucleation using a coiled electrode(or PkEEP) first described in 2006. These authors’ unique contribution to the literature is to compare electrosurgical endoscopic enucleation with open prostatectomy in large prostates (>80 g by TRUS) in a randomized trial and provide Level 1 evidence for this technique. The groups were well-matched preoperatively and were equivalent in terms of operating time, weight of tissue retrieved and postoperative variables up to 12-month follow-up. Significant advantages were noted in perioperative outcomes in favour of the endoscopic technique, particularly those outcomes related to blood loss and subsequent hospital stay. Although not specifically addressed, it is highly likely that substantial cost savings were also achieved and patients returned to normal activities sooner with the endoscopic approach.
Endoscopic enucleation for very large prostates using the Holmium laser as the energy source, was first described over a decade ago. Holmium laser enucleation of the prostate (HoLEP) has been compared with open prostatectomy in two randomized trials (Eur Urol 2006, Eur Urol 2008) and similar advantages were noted to those of BPEP in the comparison. The next question is, therefore, which of the endoscopic enucleation techniques is superior? Before this question can be answered, we need to separate those techniques that merely resect large tissue fragments (a ‘mega-resection’), and call themselves ‘enucleation’, from those that truly involve complete enucleation of the anatomical lobes using established surgical planes. HoLEP clearly falls into the latter category but electrosurgical methods may or may not because the actual surgical plane, with both electrosurgery and continuous laser wavelengths such as the Thulium : YAG, 532 nm and Diode lasers, is more difficult to achieve and follow. Exponents of these alternative energy sources perform a variety of different procedures, ranging from resection and vaporization hybrids through to a true enucleation technique, all under the banner of ‘enucleation’. For example, ‘green EP’ with a side-firing fibre, can be a true enucleation technique if blunt dissection is also employed or a ‘mega-resection’ if the laser energy is merely used to cut off the lobe as a single large fragment. The use of the morcellator is also variable, with some authors instead reverting to the resectoscope to resect the lobes while they remain attached at the bladder neck.
The movement back to enucleation techniques, which also yield tissue for analysis, is partly attributable to the desire to detect transition zone cancers but, more importantly, to address the inadequacy of other endoscopic procedures in treating the growing number of huge glands confronting the urologist as a long-term result of the rise of medical therapy. Traditionally, glands > 80–100 g have been thought to be unsuitable for TURP and morbidity becomes significant although laser techniques such as 532 nm vaporization with high-powered devices have been employed in large glands, albeit with prolonged operating times. Unsurprisingly, the retropubic and suprapubic techniques have also been re-visited by robotic surgeons but with more morbidity than HoLEP, although this will probably improve.
Endoscopic enucleation seems to be here to stay with mounting scientific and popular support. It remains to be seen which variation will gain ascendancy in the coming years, but commercial considerations rather than science will probably be the major determining factor.
Peter J. Gilling
Department of Urology, Tauranga Hospital, Tauranga, New Zealand