Editorial: Sexual function in patients undergoing combination treatment with α1‐adrenoceptor antagonists and 5α‐reductase inhibitors – a step forward in a still‐open debate
Combination treatment with α1‐adrenoceptor antagonists and 5α‐reductase inhibitors (5ARIs) is recommended in men with moderate‐to‐severe LUTS and risk of disease progression 1, 2. These drugs can improve symptoms as well as urodynamic markers of BOO 3, 4. Despite the clinical benefits, the potential negative impact of these drugs on sexual function is of major concern, and may be cause for treatment discontinuation. Additionally, in everyday clinical practice, the incidence of sexually‐related adverse events is often perceived to be higher than that reported in clinical trials, and clinicians may consequently be reluctant to prescribe these drugs in younger, sexually active patients 5. Evidence from the literature in this area, however, is low‐level, controversial and inconclusive. Notably, in most clinical studies on combination treatment, assessment of sexual function is based only on the reported incidence of sexually‐related adverse events; a non‐quantitative method that can be biased by the subjective burden of suffering, by a patient’s misinterpretation of symptoms and his propensity to mention them during follow‐up visits.
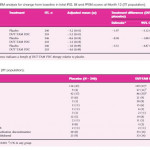
Roehrborn et al. 1 investigated the impact of a fixed‐dose combination of the 5ARI dutasteride 0.5 mg and the α1‐adrenoceptor antagonist tamsulosin 0.4 mg therapy on sexual function in sexually active men with LUTS, secondary to BPH 1. The authors designed a prospective, randomized, placebo‐controlled study and adopted, for the first time in this setting, the Men’s Sexual Health Questionnaire (MSHQ). Overall, 489 patients, with a mean age of 65.5 years, an IPSS ≥12 and a prostate volume ≥30 mL were randomized to receive combination therapy (n = 243) or placebo (n = 246) for 12 months. Change in sexual function from baseline to month 12, as measured by a change in total MSHQ score, was the primary endpoint of the study. Change from baseline in the MSHQ erection, ejaculation and satisfaction domain scores were among the secondary endpoints. The authors found a statistically significant decrease in the total MSHQ score in the active treatment group compared with placebo at all post‐treatment visits (months 1,3, 6, 9 and 12), indicating a worsening of sexual function 1. The magnitude of the total MSHQ reduction was greater at month 6 and remained substantially unchanged beyond this time point. This change was driven largely by the change in the score for the ejaculatory domain, which showed a similar temporal trend. Changes in terms of the overall satisfaction domain, although statistically significant, were judged to be numerically small and therefore unlikely to be clinically relevant. Changes in terms of erectile domain score were not statistically significant.
The major methodological strength of this study was the adoption of the MSHQ, a clinically validated questionnaire designed to assess quantitatively multiple domains of sexual function, namely erectile function, ejaculatory function and sexual satisfaction. Findings are relevant from both a pathophysiological and clinical viewpoint. Indeed, the temporal trend that characterizes the deterioration of ejaculatory function and therefore the total MSHQ score implies the involvement of both drugs in this process. From a clinical point of view the study provides additional data to counsel patients requiring combination therapy about the deleterious effects on sexual function and particularly on ejaculatory function. The main limitations of the study, as acknowledged by the authors, is the lack of long‐term follow‐up. Indeed, a recent meta‐analysis showed a positive correlation between duration of therapy with 5ARIs and incidence of sexual dysfunction, with long‐term exposure (≥1 year) being associated with a significantly higher risk 6. Consequently, conclusive data about erectile function cannot be drawn based on the results from the present 1‐year‐long study. Additionally, the authors do not report on possible changes in sexual desire. This aspect deserves future investigation as the risk of decreased libido has been reported to be statistically significant in patients assuming therapy with 5ARIs 6. Finally, results from clinical trials do not always correspond to everyday clinical practice, as patient selection for therapies in the real world is often different with respect to inclusion criteria adopted in clinical trials. Specifically, patients who receive therapy with 5ARIs (alone or in combination) in everyday clinical practice are often older than the patients who were enrolled in the present study and in other clinical trials and therefore may have comorbidities that could contribute to the development of sexual side effects during treatment 5.
- 1 Roehrborn CG, Manyak MJ, Palacios‐Moreno JM et al. A prospective randomised placebo‐controlled study of the impact of dutasteride/tamsulosin combination therapy on sexual function domains in sexually active men with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH). BJU Int 2018; 121: 647–58
- 2 Gratzke C, Bachmann A, Descazeaud A et al. EAU guidelines on the assessment of non‐neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol2015; 67: 1099–109
- 3 Fusco F, Creta M, Imperatore V et al. Benign prostatic obstruction relief in patients with lower urinary tract symptoms suggestive of benign prostatic enlargement undergoing endoscopic surgical procedures or therapy with alpha‐blockers: a review of urodynamic studies. Adv Ther2017; 34: 773–83
- 4 Matsukawa Y, Takai S, Funahashi Y et al. Effects of withdrawing α1‐blocker from combination therapy with α1‐blocker and 5α‐reductase inhibitor in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a prospective and comparative trial using urodynamics. J Urol 2017; 198: 905–12
- 5 Fusco F, Arcaniolo D, Creta M et al. Demographic and comorbidity profile of patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia in a real‐life clinical setting: Are 5‐alpha‐reductase inhibitor consumers different? World J Urol 2015; 33: 685–9
- 6 Liu L, Zhao S, Li F et al. Effect of 5α‐reductase inhibitors on sexual function: a meta‐analysis and systematic review of randomized controlled trials. J Sex Med 2016; 13: 1297–310