Editorial: Getting to the right biopsy in the right patient at the right time
Guidelines now recommend performing multiparametric MRI (mpMRI) and targeted prostate biopsies in men with a history of prior negative biopsy and continued concern for significant cancer. This new approach to prostate re-biopsy is aimed at improving prostate cancer detection. However, several important clinical factors may help clinicians’ fine-tune the process of repeated prostate biopsy. In this month’s issue of the BJUI, Hansen et al. [1] present a multicentre study of patients with prior negative TRUS biopsy undergoing MRI/TRUS-fusion transperineal biopsy.
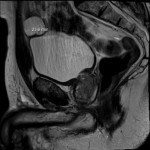
In the study, 487 men undergo mpMRI and transperineal biopsy with detection of clinically significant (Gleason score 7–10) cancer as the primary outcome. Several factors are evaluated to compare cancer detection rates, including systematic biopsies, targeted biopsies, PSA density (PSAD), and Prostate Imaging Reporting and Data System (PI-RADS) version 1 score. From their cohort, a suspicious lesion (PIRADS 3–5) was identified in 343 (70%) patients. Prostate cancer was detected in 249 (51%), with 149 (31%) having Gleason score 7–10 cancer. Potentially missed significant cancers from the anterior prostate were found in 27% (40/149). Cancer was detected in 28% (40/144) of patients with PI-RADS 1–2 lesions, with 8% (11/144) being Gleason score 7–10. For patients with PI-RADS 3–5 lesions, cancer was identified in 61% (209/343) with 40% (138/343) being Gleason score 7–10. For patients with PI-RADS 3–5 lesions, systematic biopsies alone failed to detect 13/138 significant cancers, while targeted biopsies missed 24/138 cancers. The combination of systematic and targeted biopsies was significantly better for Gleason score 7–10 prostate cancer detection than either alone. The addition of a PSAD threshold of 0.15 ng/mL/mL for the detection of Gleason score 7–10 resulted in a significant improvement in the area under the curve (0.846) of the receiver operating characteristic curve for PSAD groups and PI-RADS score.
Getting the right biopsy: In this study [1], patients with a prior negative TRUS biopsy underwent TRUS-fusion transperineal biopsy. Having two approaches to prostate biopsy can be advantageous when evaluating men with prior negative biopsies. Historical studies have found comparable prostate cancer detection between transrectal and transperineal biopsies for men undergoing both initial biopsy [2] and saturation re-biopsy [3]. However, the detection of anterior lesions has remained a persistent challenge from the transrectal approach. As in the current study [1], use of transperineal biopsy can detect cancer in up to 30% of tumours that would otherwise be missed on extended template TRUS biopsy [4]. Although attempts to reach anterior lesions from the transrectal approach may be feasible [5], the transperineal approach is felt to provide better sampling in comparison [6].
Getting the right patient: Patient-specific factors such as PI-RADS lesions 3–5 and PSAD have become increasing utilised for stratifying patients who may benefit from additional biopsies using image guidance. As the authors suggest, patients with negative imaging may consider deferring repeat biopsy, particularly those with reassuring PSADs (<0.15 ng/mL/mL). In their study [1], only 4% (6/144) of men with negative mpMRI and a PSAD of <0.15 ng/mL/mL harboured clinically significant cancer (five Gleason score 3 + 4 and one Gleason score 8). Patients with concerning PSAD, but negative mpMRI and those with lesions identified in the peripheral zone could have the option to undergo repeated, fusion-directed TRUS or transperineal biopsy. For patients with lesions identified in the anterior prostate, a transperineal prostate biopsy may provide the highest detection rate.
At the right time: Now that high quality prostate MRI is becoming more widely available; men with a prior negative biopsy should strongly consider the benefit of repeated biopsy after prostate imaging. In addition to identifying suspicious lesions, calculating PSAD has been found to improve the likelihood of detecting clinically significant prostate cancer. Without additional testing, a personalised biopsy plan can be created.
A thorough discussion of the prescribed biopsy approach and the likelihood of detecting a significant cancer is the final step to the right biopsy in the right patient at the right time.